College of Nursing, Pusan National University, Yangsan, Korea
Copyright © 2016 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Characteristics | Categories | Total | Control (n=25) | Exp. (n=16) | x2 or t (p) | |
|---|---|---|---|---|---|---|
| n (%) or M±SD | D n (%) or M±SD | n (%) or M±SD | ||||
| Age (year) (range 40~77) | <65 | 30 (73.2) | 17 (68.0) | 13 (81.3) | 0.87 (.287)§ | |
| ≥65 | 11 (26.8) | 8 (32.0) | 3 (18.8) | -0.86 (.393) | ||
| 58.02±12.04 | 56.72±14.38 | 60.06±6.97 | ||||
| Gender | Male | 30 (73.2) | 17 (68.0) | 13 (81.3) | 0.87 (.478)§ | |
| Female | 11 (26.8) | 8 (32.0) | 3 (18.8) | |||
| Spouse | No | 2 (4.9) | 0 (0.0) | 2 (12.5) | 3.29 (.146)§ | |
| Yes | 39 (95.1) | 25 (100.0) | 14 (87.5) | |||
| Level of education | ≤Junior high school | 9 (22.0) | 7 (28.0) | 2 (12.5) | 6.61 (.085) | |
| High school | 13 (31.7) | 5 (20.0) | 8 (50.0) | |||
| ≥College | 19 (46.3) | 13 (52.0) | 6 (37.5) | |||
| Regular exercise | No | 41 (100.0) | 25 (100.0) | 16 (100.0) | ||
| Monthly household income (10,000 won) | <100 | 4 (9.8) | 2 (8.0) | 2 (12.5) | 0.32 (.854) | |
| 100~199 | 7 (17.1) | 4 (16.0) | 3 (18.8) | |||
| ≥200 | 30 (73.2) | 19 (76.0) | 11 (68.8) | |||
| Left ventricular ejection fraction (%) | 31.15±6.92 | 31.88±6.98 | 30.00±6.88 | 0.85 (.403) | ||
| NYHA class | II | 36 (87.8) | 22 (88.8) | 14 (87.5) | 0.01 (>.999)§ | |
| III | 5 (12.2) | 3 (12.0) | 2 (12.5) | |||
| Comorbidity | No | 16 (39.0) | 11 (44.0) | 5 (31.3) | 0.67 (.519)§ | |
| Yes† | 25 (61.0) | 14 (56.0) | 11 (68.8) | |||
| Hypertension | 25 (100.0) | 14 (56.0) | 11 (44.0) | |||
| Diabetes mellitus | 6 (24.0) | 2 (8.0) | 4 (16.0) | |||
| Etc.‡ | 7 (28.0) | 3 (12.0) | 4 (16.0) | |||
| Medication | Beta-blocker | Yes | 35 (85.4) | 21 (84.0) | 14 (87.5) | 0.10 (>.999)§ |
| No | 6 (14.6) | 4 (16.0) | 2 (12.5) | |||
| ACE inhibitor | Yes | 29 (70.7) | 17 (68.0) | 12 (75.0) | 0.23 (.734)§ | |
| No | 12 (29.3) | 8 (32.0) | 4 (25.0) | |||
| Diuretics | Yes | 31 (75.6) | 19 (76.0) | 12 (75.0) | 0.01 (>.999)§ | |
| No | 10 (24.4) | 6 (24.0) | 4 (25.0) | |||
| Physical activity (MET-minutes/week) | Inactive | 26 (63.4) | 18 (72.0) | 8 (50.0) | 3.11 (.211) | |
| Minimally active | 11 (26.8) | 6 (24.0) | 3 (31.3) | |||
| HEPA | 4 (9.8) | 1 (2.4) | 3 (18.8) |
| Characteristics | Total | Cont. (n=25) | Exp. (n=16) | t (p) | ||
|---|---|---|---|---|---|---|
| M±SD | M±SD | Z† (p) | M±SD | Z† (p) | ||
| Dyspnea-fatigue symptoms | 5.90±1.88 | 6.20±1.78 | 0.967 (.307) | 5.44±2.00 | .943 (.336) | 1.28 (.210) |
| Daily activities (KASI) | 34.76±11.75 | 35.02±11.57 | 0.646 (.798) | 34.35±12.40 | .817 (.517) | 0.18 (.861) |
| Walking ability (6MWD; m) | 337.32±71.03 | 339.20±79.11 | 1.019 (.251) | 334.38±58.53 | .388 (.998) | 0.21 (.835) |
| HRQoL | 69.80±11.69 | 72.54±11.77 | 1.052 (.219) | 65.53±10.53 | .823 (.508) | 1.94 (.060) |
| Characteristics | Pretest | Posttest | t (p) |
|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | ||
| Walking compliance (MET-minute/week)† | |||
| <825 | 15 (93.8) | 0 (0.0) | |
| ≥825 | 1 (6.3) | 16 (100.0) | |
| Physical activity‡ | 2110.50±1693.79 | 3611.25±2513.51 | 3.45 (.041) |
| Inactive | 8 (50.0) | 0 (0.0) | |
| Minimally active | 5 (31.3) | 12 (75.0) | |
| HEPA | 3 (18.8) | 4 (25.0) | |
| Variables | Groups | Pretest | Posttest | t (p)† | Mean differences | t (p) |
|---|---|---|---|---|---|---|
| M±SD | M±SD | |||||
| Global perceived improvement in dyspnea-fatigue | Cont. (n=25) | - | 4.08±0.57 | 8.63 | ||
| Exp. (n=16) | - | 2.56±0.51 | (<.001)‡ | |||
| Daily activities (KASI) | Cont. (n=25) | 35.02±11.57 | 35.38±12.00 | 0.60 (.553) | 0.36±3.02 | -4.92 (<.001) |
| Exp. (n=16) | 34.35±12.40 | 39.80±13.03 | 6.16 (<.001) | 5.45±3.53 | ||
| Walking ability (6MWD, m) | Cont. (n=25) | 339.20±79.11 | 349.60±78.87 | -1.64 (.114) | 10.40±31.69 | -5.66 (<.001) |
| Exp. (n=16) | 334.38±58.53 | 403.13±52.50 | -8.23 (<.001) | 68.75±33.04 | ||
| Health related quality of life | Cont. (n=25) | 72.54±11.77 | 72.77±12.48 | -0.37 (.709) | 0.23±3.04 | -9.05 (<.001) |
| Exp. (n=16) | 65.53±10.53 | 79.79±7.340 | -9.99 (<.001) | 14.26±5.71 |

Reinforced Walking Exercise Program
| Categories | Contents | Time |
|---|---|---|
| 1) Preparation | (1) Perform physical assessment (Vital sign & SpO2) | 10 min |
| (2) Instruct how to use pedometer: Mode & Reset | ||
| (3) Offer exercise diary & teach how to use the diary: Recording number of steps, duration of exercise, weekly frequency, heart rate, and dyspnea/fatigue borg scale | ||
| 2) Goal setting | (1) Perform walking exercise using the pedometer | 5 min |
| (2) Start from 5,000 steps & 10% increase/week | ||
| Start from 1 day/week → 5 days/week | ||
| 1st week: 5,000 steps & 1 day/week | ||
| 2nd week: 6,000 steps & 2 days/week | ||
| 3rd week: 7,000 steps & 3 days/week | ||
| 4th week: 8,000 steps & 4 days/week | ||
| 5th week: 9,000 steps & 5 days/week | ||
| 6th week: 10,000 steps & 5 days/week | ||
| 7~12th week: maintain 10,000↑steps & 5 days/week | ||
| (3) Maintain symptom of dyspnea/fatigue based on borg scale 12~13 point, maximum heart rate 60~70% | ||
| 3) Feedback | (1) Check pedometer data and incomplete data | 5 min |
| (2) Mutually set a weekly goal of walking. | ||
| (3) Reinforce maintenance of walking exercise | ||
| → through telephone call: | ||
| 1st~6th week=once a week | ||
| 7~12th week=every other week | ||
| → by text message: 2 days/week |
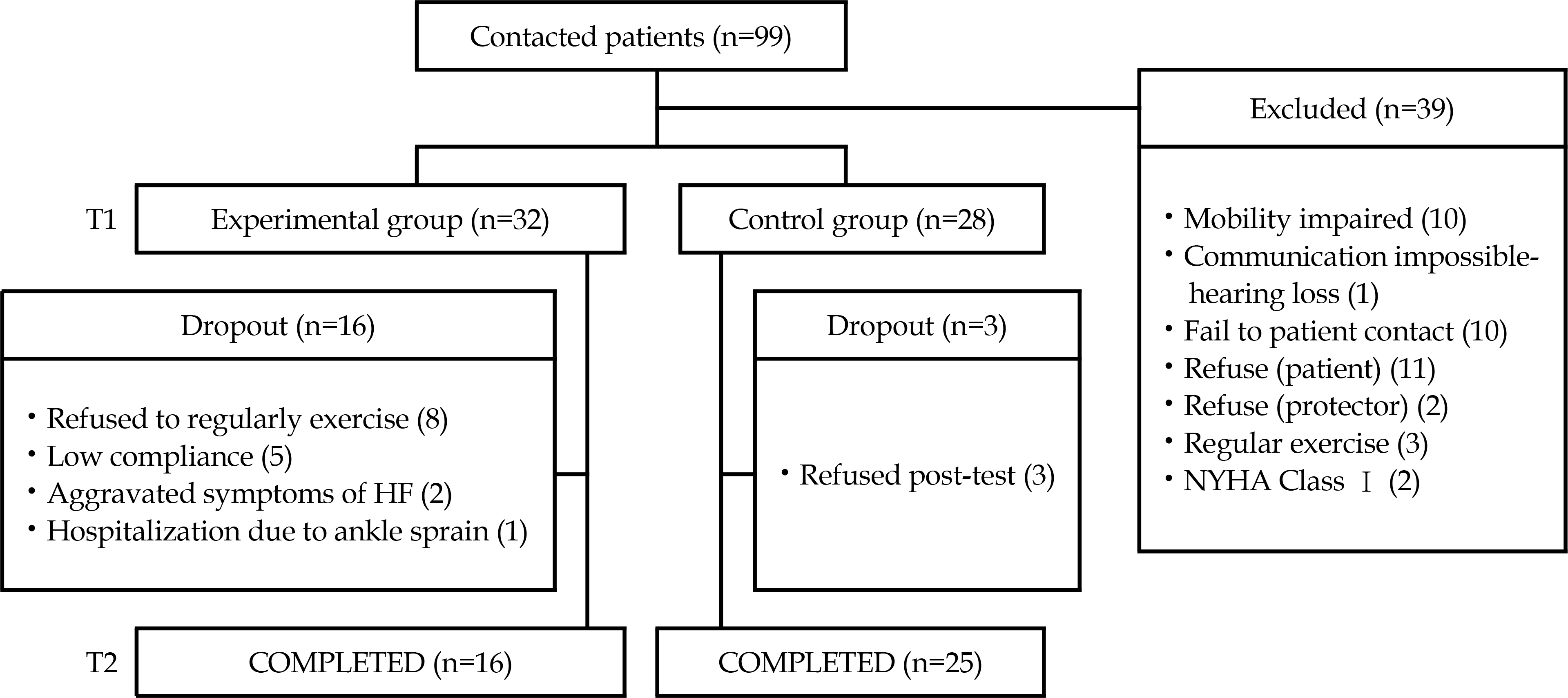
Characteristics and Homogeneity Test between Control and Experimental Groups (N=41)
| Characteristics | Categories | Total | Control (n=25) | Exp. (n=16) | x2 or t (p) | |
|---|---|---|---|---|---|---|
| n (%) or M±SD | D n (%) or M±SD | n (%) or M±SD | ||||
| Age (year) (range 40~77) | <65 | 30 (73.2) | 17 (68.0) | 13 (81.3) | 0.87 (.287) |
|
| ≥65 | 11 (26.8) | 8 (32.0) | 3 (18.8) | -0.86 (.393) | ||
| 58.02±12.04 | 56.72±14.38 | 60.06±6.97 | ||||
| Gender | Male | 30 (73.2) | 17 (68.0) | 13 (81.3) | 0.87 (.478) |
|
| Female | 11 (26.8) | 8 (32.0) | 3 (18.8) | |||
| Spouse | No | 2 (4.9) | 0 (0.0) | 2 (12.5) | 3.29 (.146) |
|
| Yes | 39 (95.1) | 25 (100.0) | 14 (87.5) | |||
| Level of education | ≤Junior high school | 9 (22.0) | 7 (28.0) | 2 (12.5) | 6.61 (.085) | |
| High school | 13 (31.7) | 5 (20.0) | 8 (50.0) | |||
| ≥College | 19 (46.3) | 13 (52.0) | 6 (37.5) | |||
| Regular exercise | No | 41 (100.0) | 25 (100.0) | 16 (100.0) | ||
| Monthly household income (10,000 won) | <100 | 4 (9.8) | 2 (8.0) | 2 (12.5) | 0.32 (.854) | |
| 100~199 | 7 (17.1) | 4 (16.0) | 3 (18.8) | |||
| ≥200 | 30 (73.2) | 19 (76.0) | 11 (68.8) | |||
| Left ventricular ejection fraction (%) | 31.15±6.92 | 31.88±6.98 | 30.00±6.88 | 0.85 (.403) | ||
| NYHA class | II | 36 (87.8) | 22 (88.8) | 14 (87.5) | 0.01 (>.999) |
|
| III | 5 (12.2) | 3 (12.0) | 2 (12.5) | |||
| Comorbidity | No | 16 (39.0) | 11 (44.0) | 5 (31.3) | 0.67 (.519) |
|
| Yes |
25 (61.0) | 14 (56.0) | 11 (68.8) | |||
| Hypertension | 25 (100.0) | 14 (56.0) | 11 (44.0) | |||
| Diabetes mellitus | 6 (24.0) | 2 (8.0) | 4 (16.0) | |||
| Etc. |
7 (28.0) | 3 (12.0) | 4 (16.0) | |||
| Medication | Beta-blocker | Yes | 35 (85.4) | 21 (84.0) | 14 (87.5) | 0.10 (>.999) |
| No | 6 (14.6) | 4 (16.0) | 2 (12.5) | |||
| ACE inhibitor | Yes | 29 (70.7) | 17 (68.0) | 12 (75.0) | 0.23 (.734) |
|
| No | 12 (29.3) | 8 (32.0) | 4 (25.0) | |||
| Diuretics | Yes | 31 (75.6) | 19 (76.0) | 12 (75.0) | 0.01 (>.999) |
|
| No | 10 (24.4) | 6 (24.0) | 4 (25.0) | |||
| Physical activity (MET-minutes/week) | Inactive | 26 (63.4) | 18 (72.0) | 8 (50.0) | 3.11 (.211) | |
| Minimally active | 11 (26.8) | 6 (24.0) | 3 (31.3) | |||
| HEPA | 4 (9.8) | 1 (2.4) | 3 (18.8) |
Exp.=experimental group; NYHA=New York Heart Association; HEPA=Health enhancing physical activity;
†Multiple responses;
‡Liver disease, osteoporosis, angina pectoris, pulmonary disease;
§Fisher's exact test.
Levels of Dyspnea-fatigue Symptoms, Daily Activities, Walking Ability and Health related QoL and Homogeneity Test (N=41)
| Characteristics | Total | Cont. (n=25) | Exp. (n=16) | t (p) | ||
|---|---|---|---|---|---|---|
| M±SD | M±SD | Z |
M±SD | Z |
||
| Dyspnea-fatigue symptoms | 5.90±1.88 | 6.20±1.78 | 0.967 (.307) | 5.44±2.00 | .943 (.336) | 1.28 (.210) |
| Daily activities (KASI) | 34.76±11.75 | 35.02±11.57 | 0.646 (.798) | 34.35±12.40 | .817 (.517) | 0.18 (.861) |
| Walking ability (6MWD; m) | 337.32±71.03 | 339.20±79.11 | 1.019 (.251) | 334.38±58.53 | .388 (.998) | 0.21 (.835) |
| HRQoL | 69.80±11.69 | 72.54±11.77 | 1.052 (.219) | 65.53±10.53 | .823 (.508) | 1.94 (.060) |
Exp.=experimental group; Cont.=control group; KASI=Korean Activity Scale/Index; 6MWD=Six-minute walk distance; HRQoL=Health related quality of life.
†Kolmogorov-Smirnove test.
Walking Compliance and Levels of Physical Activity in Experimental Group (N=16)
| Characteristics | Pretest | Posttest | t (p) |
|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | ||
| Walking compliance (MET-minute/week) |
|||
| <825 | 15 (93.8) | 0 (0.0) | |
| ≥825 | 1 (6.3) | 16 (100.0) | |
| Physical activity |
2110.50±1693.79 | 3611.25±2513.51 | 3.45 (.041) |
| Inactive | 8 (50.0) | 0 (0.0) | |
| Minimally active | 5 (31.3) | 12 (75.0) | |
| HEPA | 3 (18.8) | 4 (25.0) | |
MET=metabolic equivalent task; HEPA=health enhancing physical activity;
†Walking 3.3 MET × 50 min/day × 5 times/week=825 MET-min/week;
‡International Physical Activity Questionnaire scoring protocol (MET-min/week).
Effects of Reinforced Walking Exercise Program on Patients Outcomes (N=41)
| Variables | Groups | Pretest | Posttest | t (p) |
Mean differences | t (p) |
|---|---|---|---|---|---|---|
| M±SD | M±SD | |||||
| Global perceived improvement in dyspnea-fatigue | Cont. (n=25) | - | 4.08±0.57 | 8.63 | ||
| Exp. (n=16) | - | 2.56±0.51 | (<.001) |
|||
| Daily activities (KASI) | Cont. (n=25) | 35.02±11.57 | 35.38±12.00 | 0.60 (.553) | 0.36±3.02 | -4.92 (<.001) |
| Exp. (n=16) | 34.35±12.40 | 39.80±13.03 | 6.16 (<.001) | 5.45±3.53 | ||
| Walking ability (6MWD, m) | Cont. (n=25) | 339.20±79.11 | 349.60±78.87 | -1.64 (.114) | 10.40±31.69 | -5.66 (<.001) |
| Exp. (n=16) | 334.38±58.53 | 403.13±52.50 | -8.23 (<.001) | 68.75±33.04 | ||
| Health related quality of life | Cont. (n=25) | 72.54±11.77 | 72.77±12.48 | -0.37 (.709) | 0.23±3.04 | -9.05 (<.001) |
| Exp. (n=16) | 65.53±10.53 | 79.79±7.340 | -9.99 (<.001) | 14.26±5.71 |
Exp.=experimental group; Cont.=control group; KASI=Korean Activity Scale/Index; 6MWD=6 minute walk distance;
†t-tests for mean differences between pretest and posttests within groups,
‡t-test for mean differences between experimental and control groups.
Exp.=experimental group; NYHA=New York Heart Association; HEPA=Health enhancing physical activity; Multiple responses; Liver disease, osteoporosis, angina pectoris, pulmonary disease; Fisher's exact test.
Exp.=experimental group; Cont.=control group; KASI=Korean Activity Scale/Index; 6MWD=Six-minute walk distance; HRQoL=Health related quality of life. Kolmogorov-Smirnove test.
MET=metabolic equivalent task; HEPA=health enhancing physical activity; Walking 3.3 MET × 50 min/day × 5 times/week=825 MET-min/week; International Physical Activity Questionnaire scoring protocol (MET-min/week).
Exp.=experimental group; Cont.=control group; KASI=Korean Activity Scale/Index; 6MWD=6 minute walk distance; t-tests for mean differences between pretest and posttests within groups, t-test for mean differences between experimental and control groups.