Assistant Professor, Department of Nursing, Dongshin University, Naju, Korea
Copyright © 2016 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Path | B | β | SE* | CR (p)† | SMC‡ | Direct effect (p) In | ndirect effect (p) | Total effect (p) |
|---|---|---|---|---|---|---|---|---|
| BPN | .409 | |||||||
| KN→BPN | 0.46 | .15 | .20 | 2.28 (.023) | .15 (.035) | - | .15 (.035) | |
| SS→BPN | 0.28 | .57 | .04 | 7.56 (<.001) | .57 (.010) | - | .57 (.010) | |
| AT | .467 | |||||||
| KN→AT | 1.13 | .25 | .27 | 4.12 (<.001) | .25 (.010) | .04 (.095) | .30 (.010) | |
| SS→AT | - | .33 (.010) | .33 (.010) | |||||
| SN→AT | 0.50 | .49 | .08 | 6.67 (<.001) | .49 (.010) | - | .49 (.010) | |
| SE→AT | - | - | - | - | - | .08 (.020) | .08 (.020) | |
| BPN→AT | 0.21 | .15 | .10 | 2.20 (.028) | .15 (.029) | .13 (.010) | .27 (.010) | |
| SN | .328 | |||||||
| SE→SN | 0.23 | .17 | .10 | 2.66 (.008) | .17 (.020) | - | .17 (.020) | |
| SS→SN | 0.22 | .31 | .06 | 3.48 (<.001) | .31 (.010) | .19 (.010) | .50 (.010) | |
| KN→SN | - | - | - | - | - | .04 (.097) | .04 (.097) | |
| BPN→SN | 0.30 | .21 | .12 | 2.44 (.015) | .21 (.031) | .06 (.020) | .26 (.010) | |
| SE | .239 | |||||||
| KN→SE | - | - | - | - | - | .05 (.095) | .05 (.095) | |
| SS→SE | 0.10 | .21 | .04 | 2.48 (.013) | .21 (.019) | .19 (.010) | .40 (.010) | |
| BPN→SE | 0.30 | .33 | .08 | 3.92 (<.001) | .33 (.010) | - | .33 (.010) | |
| INT | .705 | |||||||
| KN→INT | -0.65 | -.13 | .28 | -2.32 (.020) | -.13 (.062) | .11 (.010) | -.02 (.858) | |
| SS→INT | -0.16 | -.19 | .06 | -2.84 (.005) | -.19 (.010) | .51 (.010) | .32 (.010) | |
| AT→INT | 0.27 | .23 | .08 | 3.38 (<.001) | .23 (.021) | - | .23 (.021) | |
| SN→INT | 0.61 | .52 | .11 | 5.76 (<.001) | .52 (.010) | .11 (.021) | .63 (.010) | |
| SE→INT | 0.81 | .45 | .10 | 7.84 (<.001) | .45 (.010) | .11 (.021) | .55 (.010) | |
| BPN→INT | - | - | - | - | - | .35 (.010) | .35 (.010) | |
| BE | .801 | |||||||
| KN→BE | 0.84 | .22 | .23 | 3.73 (<.001) | .22 (.010) | -.04 (.452) | .17 (.023) | |
| SS→BE | 0.12 | .19 | .04 | 3.32 (<.001) | .19 (.010) | .26 (.010) | .45 (.010) | |
| AT→BE | -0.13 | -.14 | .06 | -2.20 (.028) | -.14 (.023) | .16 (.021) | .01 (.900) | |
| SN→BE SE→BE | - 0.32 | - .23 | - .09 | - 3.58 (<.001) | - .23 (.010) | .36 (.010) .36 (.010) | .35 (.010) .59 (.010) | |
| SE→BE BPN BE | 0.32 - | .23 - | .09 - | 3.58 (<.001) - | .23 (.010) - | .36 (.010) .27 (.010) | .59 (.010) .27 (.010) | |
| BPN→BE | - | - | - | - | - | .27 (.010) | .27 (.010) | |
| INT→BE | 0.52 | .67 | .06 | 8.59 (<.001) | .67 (.010) | - | .67 (.010) | |

Descriptive Statistics for Latent Variables and Measured Variables (N=476)
| Latent variables | Measured variables | Range | M±SD | Min-Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|
| KN | 0~20 | 16.47±2.69 | 7~20 | -0.90 | 0.46 | |
| Knowledge 1 | 0~10 | 8.34±0.53 | 3~10 | -0.94 | 0.48 | |
| Knowledge 2 | 0~10 | 8.12±1.59 | 2~10 | -0.84 | 0.34 | |
| SS | 18~90 | 70.33±12.05 | 21~90 | -0.68 | 1.06 | |
| Medical staff support | 8~40 | 31.82±5.27 | 8~40 | -0.68 | 1.55 | |
| Family support | 10~50 | 38.50±8.47 | 12~50 | -0.77 | 0.29 | |
| BPN | 18~90 | 63.06±9.83 | 18~90 | -0.26 | 0.63 | |
| Autonomy | 6~30 | 22.27±0.96 | 6~30 | -0.28 | 0.11 | |
| Competency | 6~30 | 18.31±4.51 | 6~30 | -0.08 | -0.26 | |
| Relatedness | 6~30 | 21.96±3.83 | 6~30 | -0.30 | 0.38 | |
| AT | 10~70 | 59.40±10.76 | 10~70 | -0.87 | 0.40 | |
| Behavioral belief | 5~35 | 28.26±5.49 | 5~35 | -1.24 | 1.79 | |
| Outcome evaluation | 5~35 | 30.64±4.80 | 5~35 | -1.46 | 2.41 | |
| SN | 10~70 | 53.52±11.96 | 10~70 | 0.13 | -0.42 | |
| Motivation to comply | 5~35 | 27.06±5.38 | 5~35 | -1.03 | 1.51 | |
| Normative belief | 5~35 | 25.97±0.58 | 5~35 | -0.67 | -0.10 | |
| SE | 9~36 | 23.90±5.45 | 9~36 | 0.09 | -0.21 | |
| Self-efficacy 1 | 4~16 | 10.82±2.70 | 4~16 | -0.06 | -0.47 | |
| Self-efficacy 2 | 5~20 | 13.07±0.30 | 5~20 | 0.16 | -0.24 | |
| INT | 10~70 | 56.92±10.33 | 12~70 | -1.38 | 2.45 | |
| Intention 1 | 5~35 | 28.01±0.23 | 6~35 | -1.30 | 2.12 | |
| Intention 2 | 5~35 | 28.71±5.30 | 5~35 | -1.44 | 2.79 | |
| BE | 16~80 | 59.65±9.88 | 30~80 | -0.20 | -0.05 | |
| Behavior 1 | 8~40 | 30.78±5.17 | 11~40 | -0.50 | 0.21 | |
| Behavior 2 | 8~40 | 28.84±5.66 | 12~40 | -0.20 | -0.28 |
KN=knowledge related to hemodialysis; SS=social support; BPN=basic psychological need; AT=attitude; SN=subjective norm; SE=self-efficacy; INT=intention; BE=sick role behavioral compliance.
Fitness Statistics of Hypothetical Structural and Modified Model (N=476)
| Goodness | χ² | p | df | χ²/df | GFI | NNFI | SRMR | CFI | RMSEA (LO90/HI90) | CAIC |
|---|---|---|---|---|---|---|---|---|---|---|
| Criteria | 2~3 | ≥.9 | ≥.9 | <1.0 | ≥.9 | .05~.08 | ||||
| Hypothetical model | 307.36 | <.001 | 94 | 3.27 | .92 | .91 | .04 | .93 | .07 (.06/.08) | 730.12 |
| Modified model | 313.99 | <.001 | 98 | 3.20 | .92 | .91 | .04 | .93 | .07 (.60/.08) | 708.09 |
GFI=goodness-of-fit index, NNFI=nonnormed fit index, SRMR=standardized root mean square residual; CFI=comparative fit index, RMSEA=root mean square error of approximation.
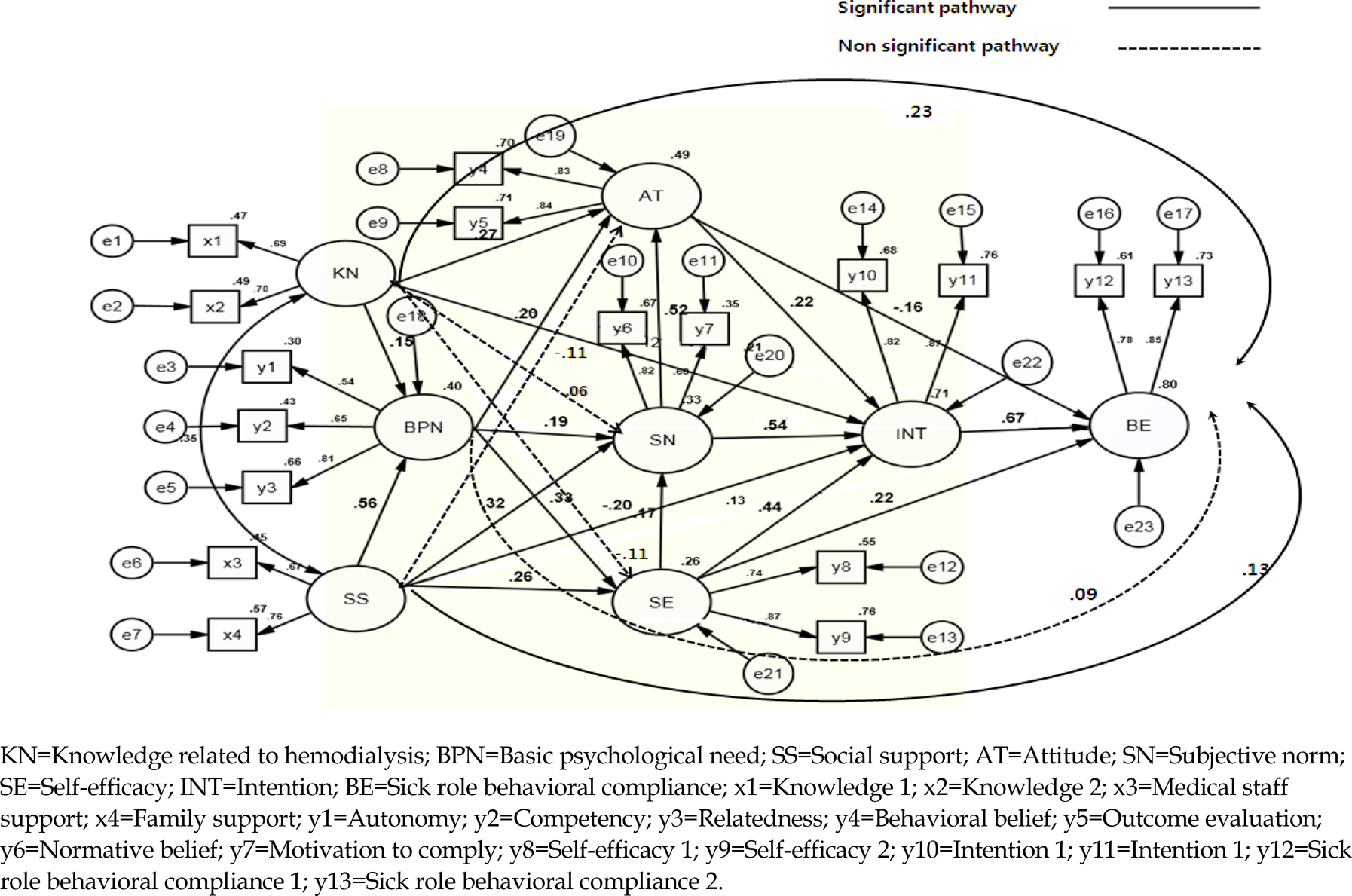
Modifie d Model wi ith Param meter Estim ate (N=476)
| Path | B | β | SE* | CR (p) |
SMC |
Direct effect (p) In | ndirect effect (p) | Total effect (p) |
|---|---|---|---|---|---|---|---|---|
| BPN | .409 | |||||||
| KN→BPN | 0.46 | .15 | .20 | 2.28 (.023) | .15 (.035) | - | .15 (.035) | |
| SS→BPN | 0.28 | .57 | .04 | 7.56 (<.001) | .57 (.010) | - | .57 (.010) | |
| AT | .467 | |||||||
| KN→AT | 1.13 | .25 | .27 | 4.12 (<.001) | .25 (.010) | .04 (.095) | .30 (.010) | |
| SS→AT | - | .33 (.010) | .33 (.010) | |||||
| SN→AT | 0.50 | .49 | .08 | 6.67 (<.001) | .49 (.010) | - | .49 (.010) | |
| SE→AT | - | - | - | - | - | .08 (.020) | .08 (.020) | |
| BPN→AT | 0.21 | .15 | .10 | 2.20 (.028) | .15 (.029) | .13 (.010) | .27 (.010) | |
| SN | .328 | |||||||
| SE→SN | 0.23 | .17 | .10 | 2.66 (.008) | .17 (.020) | - | .17 (.020) | |
| SS→SN | 0.22 | .31 | .06 | 3.48 (<.001) | .31 (.010) | .19 (.010) | .50 (.010) | |
| KN→SN | - | - | - | - | - | .04 (.097) | .04 (.097) | |
| BPN→SN | 0.30 | .21 | .12 | 2.44 (.015) | .21 (.031) | .06 (.020) | .26 (.010) | |
| SE | .239 | |||||||
| KN→SE | - | - | - | - | - | .05 (.095) | .05 (.095) | |
| SS→SE | 0.10 | .21 | .04 | 2.48 (.013) | .21 (.019) | .19 (.010) | .40 (.010) | |
| BPN→SE | 0.30 | .33 | .08 | 3.92 (<.001) | .33 (.010) | - | .33 (.010) | |
| INT | .705 | |||||||
| KN→INT | -0.65 | -.13 | .28 | -2.32 (.020) | -.13 (.062) | .11 (.010) | -.02 (.858) | |
| SS→INT | -0.16 | -.19 | .06 | -2.84 (.005) | -.19 (.010) | .51 (.010) | .32 (.010) | |
| AT→INT | 0.27 | .23 | .08 | 3.38 (<.001) | .23 (.021) | - | .23 (.021) | |
| SN→INT | 0.61 | .52 | .11 | 5.76 (<.001) | .52 (.010) | .11 (.021) | .63 (.010) | |
| SE→INT | 0.81 | .45 | .10 | 7.84 (<.001) | .45 (.010) | .11 (.021) | .55 (.010) | |
| BPN→INT | - | - | - | - | - | .35 (.010) | .35 (.010) | |
| BE | .801 | |||||||
| KN→BE | 0.84 | .22 | .23 | 3.73 (<.001) | .22 (.010) | -.04 (.452) | .17 (.023) | |
| SS→BE | 0.12 | .19 | .04 | 3.32 (<.001) | .19 (.010) | .26 (.010) | .45 (.010) | |
| AT→BE | -0.13 | -.14 | .06 | -2.20 (.028) | -.14 (.023) | .16 (.021) | .01 (.900) | |
| SN→BE SE→BE | - 0.32 | - .23 | - .09 | - 3.58 (<.001) | - .23 (.010) | .36 (.010) .36 (.010) | .35 (.010) .59 (.010) | |
| SE→BE BPN BE | 0.32 - | .23 - | .09 - | 3.58 (<.001) - | .23 (.010) - | .36 (.010) .27 (.010) | .59 (.010) .27 (.010) | |
| BPN→BE | - | - | - | - | - | .27 (.010) | .27 (.010) | |
| INT→BE | 0.52 | .67 | .06 | 8.59 (<.001) | .67 (.010) | - | .67 (.010) | |
SE=standard error; KN=knowledge related to hemodialysis; BPN=basic psychological need; SS=social support; AT=attitude; SN=subjective norm; SE=self-efficacy; INT=intention; BE=sick role behavioral compliance;
†Critical ratio;
‡Squared multiple correlation.
KN=knowledge related to hemodialysis; SS=social support; BPN=basic psychological need; AT=attitude; SN=subjective norm; SE=self-efficacy; INT=intention; BE=sick role behavioral compliance.
GFI=goodness-of-fit index, NNFI=nonnormed fit index, SRMR=standardized root mean square residual; CFI=comparative fit index, RMSEA=root mean square error of approximation.
SE=standard error; KN=knowledge related to hemodialysis; BPN=basic psychological need; SS=social support; AT=attitude; SN=subjective norm; SE=self-efficacy; INT=intention; BE=sick role behavioral compliance; Critical ratio; Squared multiple correlation.

