Abstract
-
Purpose
This study evaluated the effectiveness of an intervention combining the abdominal draw-in maneuver (ADIM) and body mechanics for nurses with chronic low back pain (LBP).
-
Methods
A non-equivalent control group pretest-posttest design was used, with data collected from August 30 to December 29, 2023. Participants were nurses experiencing chronic LBP (≥3 months) from a university hospital. Participants were allocated by ward units, with the experimental group (n=30) enrolled first, followed by the control group (n=30). The experimental group received ADIM and body mechanics training, performed ADIM exercises three times weekly for 6 weeks, and received daily text reminders. Exercise adherence and body mechanics usage were monitored weekly. The control group received educational materials upon request after study completion. Outcomes included LBP intensity, LBP disability, lumbar flexibility, and body mechanics performance, analyzed using SPSS version 27.0 through descriptive statistics, the chi-squared test, the Fisher exact tests, the independent t-test, the Mann-Whitney U test, and analysis of covariance.
-
Results
Compared to the control group, the experimental group showed significant reductions in LBP intensity (Z=4.65, p<.001) and LBP disability (F=7.04, p=.010), as well as improvements in lumbar flexibility (t=6.15, p<.001) and body mechanics performance (t=6.91, p<.001).
-
Conclusion
The intervention effectively alleviated LBP, reduced disability due to LBP, and improved lumbar flexibility and body mechanics performance. Thus, integrating ADIM with body mechanics may represent a practical and beneficial approach for reducing pain and enhancing functional outcomes among nurses experiencing chronic LBP in clinical settings.
-
Key Words: Abdominal core; Exercise therapy; Low back pain; Nurses
INTRODUCTION
Nurses face a high risk of musculoskeletal disorders due to the physically demanding nature of patient care and clinical procedures [
1]. Among these disorders, low back pain (LBP) is the most common. Previous studies reported that over 50% of nurses experience LBP lasting at least one day per year, and more than 30% suffer chronic LBP persisting for more than one week or recurring at least monthly [
2]. Additionally, more than 50% of nurses reported experiencing LBP rated 4 or higher on a Visual Analog Scale [
3]. LBP is not only a source of physical discomfort but is also linked to decreased job satisfaction, reduced work efficiency, and increased absenteeism, making it a significant occupational health concern [
1,
3,
4].
LBP in nurses commonly results from patient handling, repetitive bending, prolonged standing, and operating heavy equipment. These activities decrease lumbar strength and flexibility, placing excessive strain on the spine [
5]. Furthermore, improper application of body mechanics intensifies lumbar stress and exacerbates LBP [
6]. Thus, strategies aimed at enhancing lumbar stability and promoting proper body mechanics are crucial for preventing and managing LBP among nurses.
As most LBP cases resolve naturally over time, non-pharmacological interventions are generally preferred over medication-based treatments [
7]. Specifically, chronic nonspecific LBP—defined as pain lasting more than 12 weeks without a clear pathoanatomical cause—is typically managed with non-pharmacological methods, unlike acute or disease-specific LBP [
7]. Although various treatments, including massage, acupuncture, manual therapy, and physical therapy, have shown effectiveness, they often require specialized equipment or visits to medical facilities, resulting in financial burden and reliance on professional intervention [
8]. In contrast, exercise-based interventions are cost-effective, sustainable, and can be performed independently without specialized equipment or professional supervision [
7].
Several studies have investigated exercise interventions for managing LBP in nurses [
9,
10]. However, these interventions often include between 5 and 22 different exercises, rendering them complex and challenging to maintain, particularly when additional equipment such as stability balls is necessary. Furthermore, shift work and fatigue limit nurses' ability to participate in structured exercise routines, with many nurses prioritizing rest or sleep over physical activity during limited free time [
11,
12]. Therefore, simpler, practical, and sustainable exercise approaches are required.
Core stabilization exercises strengthen deep spinal muscles, enhance lumbar stability and flexibility, increase range of motion, and reduce LBP disability, making them particularly beneficial for managing chronic LBP [
13]. Specifically, activating deep core muscles helps prevent persistent pain and muscle atrophy in chronic LBP patients [
14]. Among core stabilization exercises, the abdominal draw-in maneuver (ADIM) has been recognized as an effective method for increasing intra-abdominal pressure by activating the transversus abdominis and internal oblique muscles. Unlike other core stabilization exercises, ADIM requires no specialized equipment or large space, making it highly practical. Previous studies reported that core stabilization exercises, including ADIM, effectively reduced LBP and LBP disability, and improved lumbar flexibility among office workers and chronic LBP patients [
13,
15,
16].
Nurses frequently experience lumbar strain resulting from patient handling and clinical procedures. Without the correct application of body mechanics, the risk of LBP significantly increases. However, structured exercise programs are challenging to adopt due to nurses' shift work and high workloads. Thus, an intervention combining ADIM with body mechanics, as a practical and easily applicable strategy, is necessary. This approach is anticipated to effectively reduce LBP and associated disability, and improve lumbar flexibility and body mechanics performance.
The aim of this study was to investigate the effects of an intervention integrating ADIM and body mechanics performance among nurses experiencing chronic LBP. The primary outcomes measured were LBP intensity and LBP disability, while the secondary outcomes were lumbar flexibility and body mechanics performance.
To achieve this objective, the following hypotheses were formulated: hypothesis 1, that nurses in the experimental group who receive the intervention consisting of ADIM and body mechanics will experience a greater reduction in LBP intensity compared to nurses in the control group; hypothesis 2, that they will experience a greater reduction in LBP disability; hypothesis 3, that they will exhibit greater improvement in lumbar flexibility; and hypothesis 4, that they will demonstrate greater improvement in body mechanics performance.
METHODS
1. Study Design
This quasi-experimental study employed a non-equivalent control group pretest-posttest design to assess the effects of an intervention incorporating the ADIM and body mechanics performance on LBP, LBP disability, lumbar flexibility, and body mechanics performance. This study was reported in accordance with the TREND (Transparent Reporting of Evaluations with Nonrandomized Designs) statement to ensure comprehensive and transparent reporting of nonrandomized intervention data.
2. Participants
The participants were nurses working three shifts in general wards at Pusan National University Hospital who experienced chronic LBP for more than 3 months—defined according to international guidelines [
17] and previous studies [
7,
13]—understood the purpose of the study, and voluntarily consented to participate. Specific inclusion and exclusion criteria were as follows:
Inclusion criteria were nurses working three shifts in general wards, with LBP lasting more than three months, and a mild to moderate pain level (Numeric Rating Scale [NRS] score 1–5). Exclusion criteria included those with lumbar conditions (e.g., herniated disc, spinal stenosis, spondylolisthesis, spinal tumors, or prior lumbar surgery), urological, gynecological, or cardiovascular diseases, pregnancy, a history of hernia, abdominal trauma or surgery, participation in a regular exercise program within the past month, and those working in specialized units such as intensive care units (ICUs) or emergency departments.
Sample size calculation was performed using G*Power version 3.1.9.4 (Heinrich-Heine University, Düsseldorf, Germany). Based on the mean and standard deviations reported in a previous study [
15], an effect size (d) of 0.81 was calculated. With an α-level of .05, statistical power (1–β) of .90, and the computed effect size of 0.81, an independent t-test analysis indicated that 26 participants per group were required. To account for potential dropouts, the sample size was increased to 30 per group. No participants withdrew during the study, and no missing data were reported, resulting in a final analytic sample of 60 participants (30 per group) (
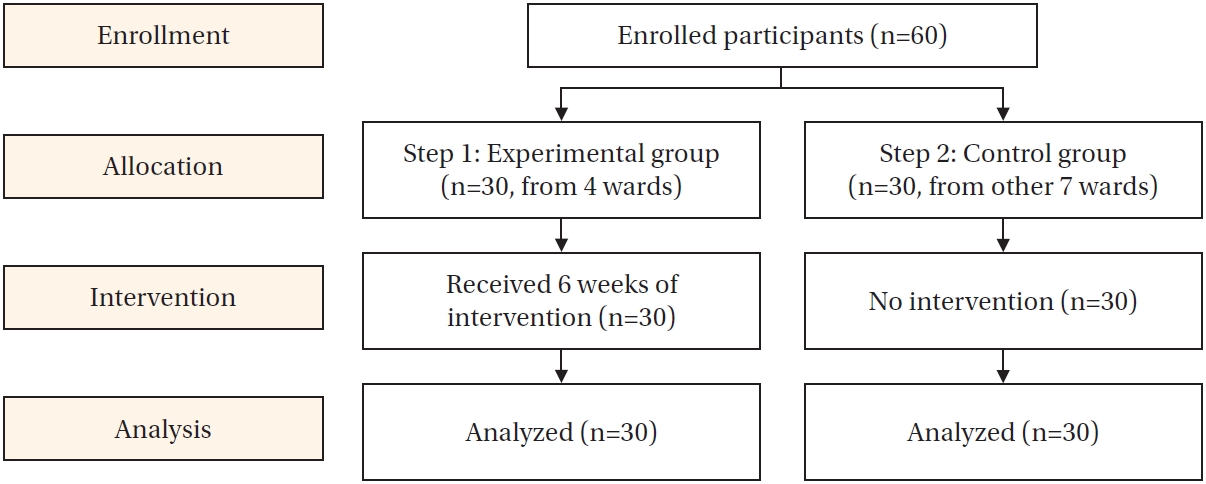
Figure 1).
1) Participant characteristics
Participant characteristics were collected using 10 items. These included seven general characteristics (sex, age, height, weight, marital status, average daily housework time, and smoking status), two work-related characteristics (department and total clinical experience), and one item regarding LBP-related experiences (hospital treatment, over-the-counter treatment, sick leave, occupational injury claims, job transfer due to LBP, or other relevant experiences). Body mass index was calculated as weight (kg) divided by height squared (m²).
2) Low back pain
LBP intensity was measured using an NRS, with participants rating their pain from 0 (no pain) to 10 (worst possible pain). Based on a previous study [
18], pain was categorized as mild (1–3), moderate (4–5), or severe (6–10).
3) LBP disability
LBP-related disability was assessed using the Korean version of the Oswestry Disability Index (KODI) [
19], adapted from the Oswestry Low Back Pain Disability Index [
20]. The original tool included 10 items: pain intensity, personal hygiene, lifting, walking, sitting, sleeping, standing, social activities, sexual activity, and traveling. The sexual activity item was excluded due to its low response rate [
19], resulting in nine items for this study.
Each item was rated on a scale of 0–5, and the scores were converted to percentages reflecting levels of disability: minimal (0%–20%), moderate (20%–40%), severe (40%–60%), very severe (60%–80%), and extreme disability (80%–100%) [
20]. The original study reported a reliability coefficient (Cronbach’s alpha) of .92, while in the current study, Cronbach’s alpha was .82.
4) Lumbar flexibility
Lumbar flexibility (in cm) was measured using a passive sit-and-reach tester (NFM-888, Nispo, Seoul, Korea), with a measurement range from –20 cm to 43 cm and a minimum measurable unit of 0.1 cm. Following a previous study [
21], participants removed their shoes, placed their feet against the vertical plane of the tester, extended their arms forward, and reached as far as possible while keeping their knees straight. Two trials were conducted, with the highest value recorded. Higher scores indicated greater lumbar flexibility.
5) Body mechanics performance
Body mechanics performance was assessed using a 7-item instrument developed by Lee [
22], evaluating nurses’ adherence to proper body mechanics during work tasks. This tool included assessment of functional posture maintenance, balance, widening of the support base, use of leg muscles, proximity to objects, utilization of body weight, and safe object-handling techniques (e.g., rolling, sliding, pushing, or pulling rather than lifting). Each item was scored on a 5-point Likert scale ranging from 1 (“never”) to 5 (“always”), with total scores between 7 and 35. Higher scores indicated greater adherence to correct body mechanics. To ensure understanding, the researchers provided clear explanations and examples. Cronbach’s alpha was .84 in the original study and .93 in this study.
The intervention administered to the experimental group comprised three components: a single session of small-group education, a 6-week period of self-training, and weekly monitoring.
1) Small-group education
The small-group educational session lasted 50 minutes and included lectures, demonstrations, and hands-on practice. Educational materials were provided in PowerPoint format (Microsoft Corp., Redmond, WA, USA) (
Table 1).
(1) Proper body mechanics
The first topic, proper body mechanics, was based on principles of postural stability and covered seven key aspects: maintaining functional posture, ensuring balance, widening the base of support, using leg muscles, approaching objects closely, using body weight, and applying proper object-handling techniques. Educational content was developed according to previous studies [
22,
23] and aligned with the measurement instruments utilized in this study. Practical examples were provided to help participants effectively apply body mechanics in clinical practice.
(2) Abdominal draw-in maneuver
The second topic, the ADIM, introduced the concept, benefits, and importance of core stabilization exercises, including specific instructions and hands-on practice. Content and training methods were based on previous literature related to core stabilization exercises [
7,
16]. Although the ADIM can be performed in standing, supine, and seated positions, prior research has indicated that the seated position is more effective than the supine position and easier to integrate into daily routines [
24]. Therefore, this study emphasized the seated position for both training and self-practice.
During the practical session, an air-pressure biofeedback device (Stabilizer, Chattanooga Group, Chattanooga, TN, USA) was used to demonstrate correct movements. This device consists of an inflatable pressure bag connected to a pressure gauge, enabling participants to monitor subtle movements of the spine or abdomen. After the demonstration, participants performed the exercise under supervision from a researcher or research assistant. A portable timer was provided to support self-directed practice.
The ADIM practice procedure using the biofeedback device was adapted from a previous study [
24] and conducted as follows: Participants sat upright on a chair with both feet flat on the floor, maintaining knees and hip joints at a 90° angle, and positioning the hips near the edge of the chair. The biofeedback device was placed under the lower back, and participants were instructed to maintain a neutral spine. The biofeedback device was inflated to 40 mmHg while monitoring the pressure gauge. Participants contracted their abdominal wall without moving their spine or pelvis, increasing the pressure reading to 50 mmHg. Participants maintained a pressure of 50 mmHg while drawing the navel inward and upward. They were advised to avoid leaning backward and to minimize tension in the thighs and pelvis.
Finally, important precautions for independent practice were explained, and participants were instructed to contact the researcher via message or phone with any inquiries or concerns.
2) Self-training
Participants performed the ADIM three times weekly for 6 weeks and practiced proper body mechanics during their daily activities. Exercise schedules were adjusted individually.
(1) Abdominal draw-in maneuver
Participants performed ADIM as follows: Participants sat upright on a chair without leaning against the backrest. The lower abdomen was drawn inward toward the spine and held for 10 seconds while maintaining relaxed breathing and avoiding movement of the pelvis or chest. After holding the contraction for 10 s, the lower abdomen was relaxed for 5 seconds. This cycle was repeated 10 times to complete a single set. Five sets were performed per day (50 repetitions) at least three times per week.
(2) Body mechanics practice
On days when exercises were not scheduled, participants received text messages reminding them of body mechanics principles. Messages included key points from educational sessions along with images or illustrations, encouraging participants to incorporate proper body mechanics into daily routines.
3) Weekly monitoring
Adherence to ADIM and body mechanics practice was monitored weekly.
(1) Abdominal draw-in maneuver
To track participation and maintain motivation, individualized exercise logs were created in image format. These logs were sent weekly, accompanied by encouraging messages supporting adherence to the intervention.
(2) Body mechanics practice
Each week, the researcher sent an online self-assessment form via text message. Participants recorded their adherence to body mechanics practices using a 5-point scale: “always,” “often,” “moderate,” “rarely,” or “never.” Self-assessment items aligned with educational content and measurement instruments. Based on participant responses, the researcher provided tailored feedback and sent additional messages reinforcing key body mechanics principles.
After drafting the educational materials and intervention procedures, content validity was reviewed by an expert panel, including a nursing professor, an orthopedic specialist, two ward nurses with experience in LBP, two physical therapists, and three exercise instructors. The materials were revised and finalized based on the panel’s feedback.
Before conducting the study, the researcher was trained by a physical therapist experienced in rehabilitation, focusing on the correct performance of the ADIM and use of the air-pressure biofeedback device. The researcher practiced under the physical therapist’s supervision and was reassessed over 20 days to ensure accuracy. Training also covered appropriate force application and effective instructional methods for participant education.
The research assistant was a licensed nurse trained in research ethics, whose duties included measuring lumbar flexibility, distributing questionnaires, and assisting with practical exercises. Training was provided in advance to ensure standardized procedures were consistently followed.
5. Study Procedure and Data Collection
Data were collected between August 30 and December 29, 2023. Participants were recruited using convenience sampling via posters and announcements through Pusan National University Hospital’s groupware and internal messaging systems. To minimize contamination risks between groups, participants were non-randomly allocated based on their ward units. The experimental group (n=30) was selected first from four wards, followed by the control group (n=30) from seven separate wards. All participants were informed of their group allocation before beginning the study.
Pre-intervention assessments were conducted before or after hospital shifts. The experimental group completed assessments in 11 small groups (2–4 participants each), arranged according to their educational session schedules. Control group participants underwent assessments individually upon recruitment. After explaining the study and obtaining written consent, participants completed the survey and submitted it in a sealed envelope. Subsequently, the researcher and research assistant measured lumbar flexibility. This entire assessment process took approximately 10 minutes per participant.
For the small-group education sessions, experimental participants were divided into 11 groups of 2–4 members. Considering shift schedules, nurses on day shifts attended the sessions after work, while evening shift nurses attended before work. After completing pre-intervention assessments, these educational sessions were conducted in a conference room at Pusan National University Hospital, equipped with a projector and sufficient space for education and practice. Printed educational materials were distributed, and PowerPoint presentations were used to teach body mechanics and the ADIM. The researcher demonstrated the techniques, after which participants practiced under supervision and received personalized feedback. Following the practical session, key intervention details and precautions were reviewed.
Exercise adherence was monitored via text messaging; participants sent an “O” after completing each session. If participants missed a session, reminders, and schedule adjustments were provided. Regular communication was maintained throughout the intervention period.
Post-intervention assessments were conducted at the hospital before or after shifts. Experimental group assessments occurred after the 6-week intervention period, while control group assessments took place 6 weeks after the pre-test, completed within 3 days considering shift schedules. Participants completed sealed surveys, and lumbar flexibility was measured again. For ethical reasons, control group participants were informed they could request educational materials or training after the study; one participant made such a request and received materials.
6. Ethical Considerations
This study was approved by the Institutional Review Board (IRB no. PNU IRB/2023_98_HR) of Pusan National University and the nursing department of Pusan National University Hospital. Participants were informed about the study’s purpose, procedures, measures for anonymity and confidentiality, secure storage of coded data, and restrictions on using data beyond the research context. Participants were also informed of their right to withdraw at any point before signing the consent form. They were advised to report any discomfort or exacerbation of symptoms during the 6-week intervention; however, no issues were reported. After the post-intervention assessments, control group participants who wished to receive educational materials or training were provided with these resources. All participants received a small token of appreciation for their involvement.
7. Data Analysis
Data were analyzed using IBM SPSS version 27.0 (IBM Corp., Armonk, NY, USA), with the significance level set at p<.05. Descriptive statistics (frequency, percentage, mean, and standard deviation) were used to summarize participant characteristics, LBP, LBP disability, lumbar flexibility, and body mechanics performance. Baseline homogeneity between the experimental and control groups was tested using the independent t-test, chi-square test, Fisher exact test, and Mann-Whitney U test. The normality of the dependent variables was evaluated using the Kolmogorov-Smirnov test. As LBP did not follow a normal distribution, the Mann-Whitney U test was used for group comparisons, while the independent t-test was performed for lumbar flexibility and body mechanics performance. Since the baseline disability scores were not homogeneous between groups, analysis of covariance (ANCOVA) was conducted to adjust for this covariate. The reliability of the measurement tools was assessed using Cronbach’s alpha coefficients.
RESULTS
1. Baseline Homogeneity Test
1) Participant characteristics
The baseline homogeneity analysis of participant characteristics revealed no significant differences between the experimental and control groups, confirming that the groups were homogeneous (
Table 2). None of the participants reported currently smoking, taking sick leave, submitting occupational injury claims, or transferring jobs due to LBP. However, some participants reported engaging in non-pharmacological treatments, such as massage and stretching, for LBP relief.
2) LBP, LBP disability, lumbar flexibility, and body mechanics performance
The baseline homogeneity tests showed no significant differences between the experimental and control groups for LBP intensity, lumbar flexibility, or body mechanics performance. However, a significant difference was found between groups in baseline LBP-related disability scores (t=2.36,
p=.022) (
Table 2).
The effectiveness of the intervention was evaluated by comparing pre- and post-intervention outcomes in both the experimental and control groups.
1) Primary outcomes
The LBP score decreased in the experimental group from 3.17±1.15 at baseline to 1.60±1.43 post-intervention, whereas the control group showed a slight increase from 2.70±1.39 to 2.77±1.63. The mean difference was –1.57±1.33 for the experimental group and 0.07±1.17 for the control group, demonstrating a statistically significant difference between groups (Z=4.65,
p<.001). Thus, hypothesis 1 was supported (
Table 3).
LBP disability scores (%) in the experimental group decreased from 15.33±7.84 to 9.63±7.08, while the control group exhibited only a slight reduction from 11.33±4.96 to 10.89±5.85. After adjusting for baseline LBP disability scores using ANCOVA, the mean differences were –5.70±6.77 in the experimental group and –0.44±4.42 in the control group, with a statistically significant group difference (F=7.04,
p=.010). Therefore, hypothesis 2 was supported (
Table 3).
2) Secondary outcomes
Lumbar flexibility improved in the experimental group, increasing from 5.03±8.55 cm to 8.88±8.12 cm, whereas the control group experienced a decrease from 8.31±8.76 cm to 7.56±8.77 cm. The mean difference was 3.85±3.42 cm in the experimental group and –0.76±2.27 cm in the control group, with a statistically significant group difference (t=6.15,
p<.001). Therefore, hypothesis 3 was supported (
Table 3).
Body mechanics performance scores improved substantially in the experimental group, from 17.10±5.45 to 28.63±3.99, while the control group showed a smaller increase, from 19.50±5.58 to 21.00±5.57. The mean differences were 11.53±5.98 for the experimental group and 1.50±5.24 for the control group, showing a statistically significant difference between groups (t=6.91,
p<.001). Thus, hypothesis 4 was supported (
Table 3).
DISCUSSION
The intervention group showed significant reductions in LBP and LBP disability, as well as notable improvements in lumbar flexibility and body mechanics performance compared to the control group. The following discussion focuses on interpreting these findings.
Regarding the primary outcomes, the participants’ average LBP score was approximately 2.9, categorizing their pain as mild (less than 4 points) according to Woo et al. [
18]. This finding aligns closely with previous research involving ICU nurses who underwent lumbar stabilization training, which reported an average LBP score of 3.02 [
10]. However, it was slightly lower than the average pain score of 3.6 reported in a study involving chronic LBP patients [
25]. Additionally, the average LBP disability score among participants in this study was 13.3%, corresponding to a “minimal disability” level based on Fairbank et al.’s classification [
20]. This disability level resembles that reported in a previous study of intensive care nurses [
10], who similarly exhibited minimal disability. Likewise, another study of chronic LBP patients reported an average KODI score of approximately 18%, also indicating minimal disability [
25]. These findings suggest that nurses in their late 20s with approximately five years of clinical experience commonly experience chronic mild LBP (NRS score ~3), although associated functional disability typically remains minimal.
Following the 6-week intervention, participants' average LBP scores decreased from approximately 3 to 1, and their LBP-related disability scores declined from around 15% to 10%. These outcomes are consistent with a previous study [
10] involving 35 ICU nurses who received body mechanics training combined with core stabilization exercises, which resulted in a 1.5-point reduction in LBP and a 6% decrease in disability. Similarly, another study [
13] of 36 nurses with chronic LBP reported a 3.4-point pain reduction and significant improvement in disability, as assessed by the Roland-Morris Disability Questionnaire. These collective findings suggest that the ADIM effectively enhances core stability, thereby alleviating both pain and functional limitations. Nurses regularly engage in activities involving forward bending, pulling, lifting, and repositioning patients; thus, proper application of body mechanics is essential for managing LBP. Teaching and implementing correct patient-handling techniques based on body mechanics principles may have significantly contributed to reducing participants’ pain levels.
Regarding the secondary outcomes, participants’ lumbar flexibility increased from approximately 5 cm at baseline to 9 cm after the 6-week ADIM and body mechanics intervention, representing an improvement of approximately 4 cm. This outcome aligns with previous studies [
9,
26,
27], which similarly reported significant lumbar flexibility improvements of 4–5 cm after core stabilization training. Improved lumbar flexibility observed in this study may be attributable to enhanced spinal stability, maintenance of proper posture, and effective application of body mechanics principles, all potentially contributing to reduced LBP. Chronic LBP is known to impair spinal flexibility and muscle strength, consequently limiting the range of motion (ROM) [
28]. Thus, evaluating lumbar flexibility and ROM is critical for assessing intervention effectiveness. However, in this study, ROM was assessed exclusively in forward-bending positions, despite potential ROM limitations also existing during rotational and extension movements.
In addition, body mechanics performance scores improved markedly from approximately 17 to 29 out of a possible 35 points following the intervention, demonstrating substantial improvement in participants’ application of body mechanics principles. This improvement surpasses findings from a previous study [
10], in which body mechanics scores increased by approximately 7 points following a single educational session combined with 6 weeks of core stabilization exercises. The greater improvement observed in the current study suggests a particularly effective intervention, possibly due to continuous reinforcement of body mechanics principles through daily text message reminders that encouraged the integration of proper techniques into daily activities. Previous research on body mechanics education has highlighted the importance of repeated training sessions at 1-week [
6] or 2-week intervals [
29]. While acquiring knowledge is important, practical application of body mechanics in daily routines is critical. Continuous motivation and frequent exposure to body mechanics principles through various media can facilitate behavioral change, thus constituting a vital component of effective body mechanics interventions.
The participants had an average age of 28.5 years and an average clinical experience of 5.8 years. This profile is comparable to previous studies involving nurses with LBP [
9,
10], where participants were also predominantly in their late 20s. However, participants in this study had slightly more clinical experience than the approximately 3-year average reported in prior studies. This difference may relate to previous findings that LBP is prevalent among nurses in their 20s [
30], whereas older nurses, who are typically more adapted to their roles and engage more frequently in managerial tasks, tend to report less LBP [
31]. Nevertheless, previous research has yielded conflicting results regarding the association between years of clinical experience and LBP, with some studies suggesting that prolonged employment increases LBP risk [
5], particularly among nurses with more than 10 years of experience [
32]. Consequently, further research including nurses with broader age ranges and varying lengths of work experience is warranted.
With respect to participants’ experiences with LBP, 70% reported no prior treatment, indicating a tendency among nurses to refrain from active LBP management. This finding aligns with a previous study by Jang and Park [
10], which similarly reported that 74% of participants had received no prior treatment. It is also consistent with another study on musculoskeletal symptoms among nurses at small- and medium-sized hospitals [
2], where 49% of nurses with LBP had not sought treatment. This reluctance to seek treatment may relate to nurses’ struggles to engage in preventive health behaviors, such as regular medical checkups and physical activity, due to demanding working hours and irregular shifts [
11]. Similarly, Ross et al. [
12] noted that nurses often recognize the importance of health management but encounter practical difficulties in adopting such behaviors because of shift work, fatigue, and family obligations, leading to low adherence rates for health-promoting practices. Therefore, practical and proactive strategies beyond raising awareness are essential to effectively support nurses in managing their LBP.
This study had several limitations. First, the LBP assessment relied on self-reported data, which could introduce subjective bias. Similarly, exercise adherence and body mechanics performance were also self-reported, limiting the objectivity of the findings. Among the outcome variables, lumbar flexibility was objectively measured; however, this study only assessed flexibility using the forward-bending position. Second, the study design did not include randomization and blinding, potentially introducing threats to internal validity. Additionally, the study protocol was not registered in a clinical trial registry, a measure that could have enhanced transparency and reduced reporting bias.
Despite these limitations, the intervention combining ADIM and body mechanics training was found to be effective in reducing LBP, alleviating functional disability, improving lumbar flexibility, and enhancing body mechanics performance among nurses. This intervention integrated ADIM with body mechanics training, enabling nurses to independently manage their LBP in everyday practice. Unlike conventional single-session training approaches, this intervention reinforced key concepts through daily text message reminders and weekly self-assessments, promoting sustained engagement. Given its practical applicability, this intervention represents a feasible and effective strategy for nurses frequently at risk for LBP due to patient handling tasks and heavy equipment use in demanding clinical settings.
CONCLUSION
This study demonstrated the effectiveness of an intervention integrating ADIM and body mechanics principles in reducing LBP and LBP-related disability while simultaneously improving lumbar flexibility and body mechanics performance among nurses experiencing chronic LBP. These findings provide practical evidence supporting a simple yet efficient intervention strategy that can easily be incorporated into daily routines, enhancing its applicability in clinical settings to prevent and manage musculoskeletal disorders among nurses. Moreover, this intervention offers a feasible self-management approach that allows nurses to decrease work-related physical strain and increase physical resilience, thereby contributing to improved nursing care quality and advancement of evidence-based nursing practices.
Future research should include more objective evaluations of intervention effectiveness, such as measurements of lumbar ROM (including rotation and extension movements) and assessments of deep muscle activation using ultrasound. Additionally, studies utilizing digital platforms, such as mobile application-based programs, are recommended to support nurses in maintaining long-term adherence to interventions.
-
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
-
AUTHORSHIP
Study conception and/or design acquisition - SC and IK; data collection and analysis - SC and SBP; interpretation of the data - SC and IK; and drafting or critical revision of the manuscript for important intellectual content - SC and SBP.
-
FUNDING
None.
-
ACKNOWLEDGEMENT
This article is a condensed form of the first author’s master’s thesis from Pusan National University.
-
DATA AVAILABILITY STATEMENT
The data can be obtained from the corresponding authors.
Figure 1.Flow diagram of study participants.
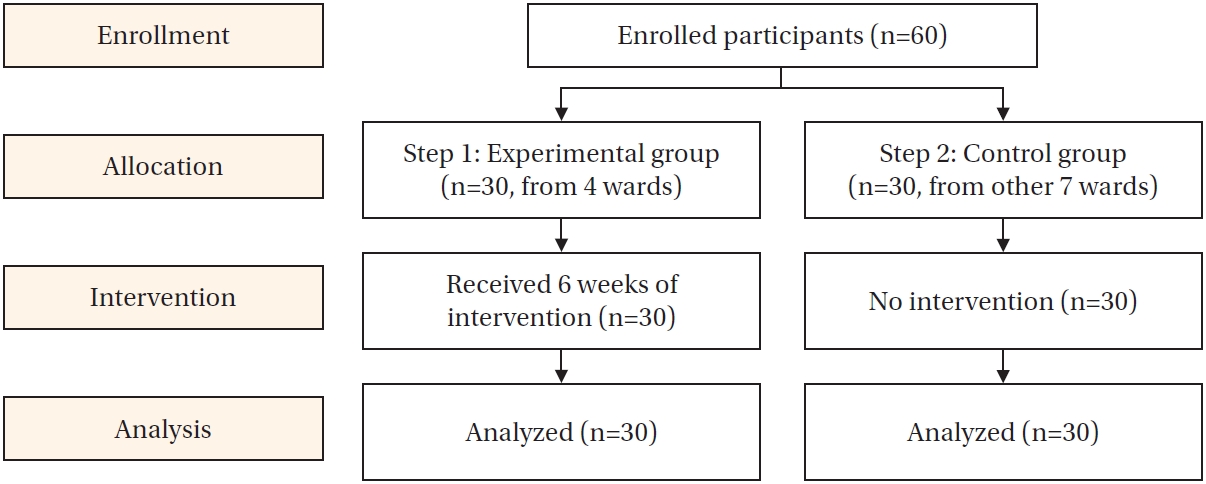
Table 1.Contents of Small Group Education
|
Category |
Contents |
Teaching Method |
Duration (minute) |
|
1 |
Proper body mechanics |
Importance and significance of body mechanics |
Lecture |
20 |
|
Proper body mechanics techniques |
|
- Maintaining functional posture |
|
- Keeping balance |
|
- Widening the base of support and lowering the center of gravity |
|
- Using leg muscles |
|
- Approaching objects closely |
|
- Utilizing body weight |
|
- Moving objects |
|
(e.g., rolling, sliding, pushing, or pulling rather than lifting) |
|
2 |
Abdominal draw-in maneuver (ADIM) |
Core stabilization exercises |
Lecture, Demonstration, and Practice |
25 |
|
- Introduction to core and deep core muscles |
|
- Definition of core stabilization exercises |
|
- Benefits and implications of core stabilization exercises |
|
What is the ADIM? |
|
How to perform the ADIM |
|
Practical training using a pressure biofeedback device |
|
3 |
Precautions |
Precautions for self-training after education |
Lecture |
5 |
Table 2.Homogeneity Test of General Characteristics of Participants and Outcome Variables in the Two Groups (N=60)
|
Characteristics |
Categories |
n (%) or M±SD |
χ² or Z or t |
p
|
|
Total (n=60) |
Exp. (n=30) |
Cont. (n=30) |
|
Sex |
Male |
1 (1.7) |
1 (3.3) |
0 (0.0) |
- |
>.999†
|
|
Female |
59 (98.3) |
29 (96.7) |
30 (100.0) |
|
|
|
Age (year) |
|
28.5±3.08 |
27.8±3.05 |
29.3±2.96 |
–1.98 |
.053 |
|
BMI (kg/m2) |
|
21.0±2.94 |
21.5±3.21 |
20.6±2.61 |
1.27 |
.209 |
|
Marital status |
Married |
8 (13.3) |
5 (16.7) |
3 (10.0) |
|
.706†
|
|
Single |
52 (86.7) |
25 (83.3) |
27 (90.0) |
|
|
|
Housework (hour) |
Almost none |
20 (33.3) |
9 (30.0) |
11 (36.7) |
- |
.934†
|
|
<1 |
32 (53.3) |
17 (56.7) |
15 (50.0) |
|
|
|
≥1 |
8 (13.3) |
4 (13.3) |
4 (13.3) |
|
|
|
Working department |
Surgery |
33 (55.0) |
19 (63.3) |
14 (46.7) |
1.68 |
.194 |
|
Internal medicine |
27 (45.0) |
11 (36.7) |
16 (53.3) |
|
|
|
Nursing career (month) |
|
69.9±37.67 |
61.3±39.51 |
78.5±34.24 |
–1.81 |
.076 |
|
LBP-related experiences‡
|
Hospital treatment |
|
|
|
|
|
|
Yes |
8 (13.3) |
5 (16.7) |
3 (10.0) |
- |
.706†
|
|
No |
52 (86.7) |
25 (83.3) |
27 (90.0) |
|
|
|
OTC treatment |
|
|
|
|
|
|
Yes |
10 (16.7) |
6 (20.0) |
4 (13.3) |
0.480 |
.488 |
|
No |
50 (83.3) |
24 (80.0) |
26 (86.7) |
|
|
|
Non-pharmacological treatment |
|
|
|
|
|
|
Yes |
4 (6.7) |
2 (6.7) |
2 (6.7) |
- |
>.999†
|
|
No |
56 (93.3) |
28 (93.3) |
28 (93.3) |
|
|
|
Outcome variables |
LBP |
2.93±1.29 |
3.17±1.15 |
2.70±1.39 |
1.39§
|
.166 |
|
LBP disability (%) |
13.33±6.81 |
15.33±7.84 |
11.33±4.96 |
2.36 |
.022 |
|
Lumbar flexibility (cm) |
6.67±8.74 |
5.03±8.55 |
8.31±8.76 |
–1.47 |
.147 |
|
Body mechanics performance |
18.30±5.60 |
17.10±5.45 |
19.50±5.58 |
–1.69 |
.097 |
Table 3.Changes in LBP, LBP Disability, Lumbar Flexibility, and Body Mechanics Performance between the Two Groups (N=60)
|
Variables |
Groups |
Pre-test |
Post-test |
Mean differences |
Z or F or t |
p
|
|
M±SD |
|
LBP |
Exp. (n=30) |
3.17±1.15 |
1.60±1.43 |
–1.57±1.33 |
4.65†
|
<.001 |
|
Cont. (n=30) |
2.70±1.39 |
2.77±1.63 |
0.07±1.17 |
|
LBP disability (%) |
Exp. (n=30) |
15.33±7.84 |
9.63±7.08 |
–5.70±6.77 |
7.04‡
|
0.01 |
|
Cont. (n=30) |
11.33±4.96 |
10.89±5.85 |
–0.44±4.42 |
|
Lumbar flexibility (cm) |
Exp. (n=30) |
5.03±8.55 |
8.88±8.12 |
3.85±3.42 |
6.15 |
<.001 |
|
Cont. (n=30) |
8.31±8.76 |
7.56±8.77 |
–0.76±2.27 |
|
Body mechanics performance |
Exp. (n=30) |
17.10±5.45 |
28.63±3.99 |
11.53±5.98 |
6.91 |
<.001 |
|
Cont. (n=30) |
19.50±5.58 |
21.00±5.57 |
1.50±5.24 |
REFERENCES
- 1. Tuna R, Eskin Bacaksiz F, Kahraman B. Compassion satisfaction, compassion fatigue, burnout, working environments, and musculoskeletal disorders among nurses. Perspect Psychiatr Care. 2022;58(4):2321-9. https://doi.org/10.1111/ppc.13063
- 2. Jung JS, Eun Y. Factors associated with musculoskeletal symptoms in small and medium sized hospital nurses. J Muscle Jt Health. 2017;24(3):159-170. https://doi.org/10.5953/JMJH.2017.24.3.159
- 3. Uhm HJ, Park HJ. Low back pain and its influencing factors among intensive care unit nurses: a cross-sectional study. J Health Info Stat. 2022;47(2):95-102. https://doi.org/10.21032/jhis.2022.47.2.95
- 4. Sorour AS, El-Maksoud MM. Relationship between musculoskeletal disorders, job demands, and burnout among emergency nurses. Adv Emerg Nurs J. 2012;34(3):272-82. https://doi.org/10.1097/TME.0b013e31826211e1
- 5. Alnaami I, Awadalla NJ, Alkhairy M, Alburidy S, Alqarni A, Algarni A, et al. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet Disord. 2019;20(1):56. https://doi.org/10.1186/s12891-019-2431-5
- 6. Moazzami Z, Dehdari T, Taghdisi MH, Soltanian A. Effect of an ergonomics-based educational intervention based on transtheoretical model in adopting correct body posture among operating room nurses. Glob J Health Sci. 2015;8(7):26-34. https://doi.org/10.5539/gjhs.v8n7p26
- 7. Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians, Denberg TD, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514-30. https://doi.org/10.7326/M16-2367
- 8. Abdelraouf OR, Abdel-Aziem AA. The relationship between core endurance and back dysfunction in collegiate male athletes with and without nonspecific low back pain. Int J Sports Phys Ther. 2016;11(3):337-44.
- 9. Kwon H, Jung H. Effect of strengthening program for nurses in relation to back pain, flexibility and muscle strength. J Korean Data Anal Soc. 2009;11(1):213-27.
- 10. Jang HM, Park HJ. Effects of a lumbar stabilization exercise program on low back pain, the Oswestry Disability Index, use of body mechanics, and lumbar strength among intensive care unit nurses. J Health Info Stat. 2022;47(3):209-16. https://doi.org/10.21032/jhis.2022.47.3.209
- 11. Kim MH, Lee JS. The health care experience of the clinical nurse in a university hospital. J Korea Acad Ind Coop Soc. 2016;17(1):209-18. http://doi.org/10.5762/KAIS.2016.17.1.209
- 12. Ross A, Bevans M, Brooks AT, Gibbons S, Wallen GR. Nurses and health-promoting behaviors: knowledge may not translate into self-care. AORN J. 2017;105(3):267-75. https://doi.org/10.1016/j.aorn.2016.12.018
- 13. Noormohammadpour P, Kordi M, Mansournia MA, Akbari-Fakhrabadi M, Kordi R. The role of a multi-step core stability exercise program in the treatment of nurses with chronic low back pain: a single-blinded randomized controlled trial. Asian Spine J. 2018;12(3):490-502. https://doi.org/10.4184/asj.2018.12.3.490
- 14. Roh JS, Park HY. The effect of balance core exercise on spinal variation, physical fitness and visual analogue scale of the middle-aged women with chronic back pain. Korean J Growth Dev. 2020;28(4):503-12. https://doi.org/10.34284/KJGD.2020.11.28.4.503
- 15. Puntumetakul R, Saiklang P, Tapanya W, Chatprem T, Kanpittaya J, Arayawichanon P, et al. The effects of core stabilization exercise with the abdominal drawing-in maneuver technique versus general strengthening exercise on lumbar segmental motion in patients with clinical lumbar instability: a randomized controlled trial with 12-month follow-up. Int J Environ Res Public Health. 2021;18(15):7811. https://doi.org/10.3390/ijerph18157811
- 16. Song HS, Jeong YS, Kim YH. The effect of abdominal drawing-in maneuver on chronic low back pain in office workers on lumbar dysfunction and balance ability. J Korean Acad Orthop Man Phys Ther. 2021;27(3):79-87. https://doi.org/10.23101/kaompt.2021.27.3.79
- 17. World Health Organization. WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings. World Health Organization report. Geneva: World Health Organization; 2023 December.
- 18. Woo A, Lechner B, Fu T, Wong CS, Chiu N, Lam H, et al. Cut points for mild, moderate, and severe pain among cancer and non-cancer patients: a literature review. Ann Palliat Med. 2015;4(4):176-83. https://doi.org/10.3978/j.issn.2224-5820.2015.09.04
- 19. Jeon CH, Kim DJ, Kim DJ, Lee HM, Park HJ. Cross-cultural adaptation of the Korean version of the Oswestry Disability Index (ODI). J Korean Soc Spine Surg. 2005;12(2):146-52. https://doi.org/10.4184/jkss.2005.12.2.146
- 20. Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271-3.
- 21. Roh JS, Jeong GY. The effects of aerobic exercise on body composition and fitness in the elderly men. Korean J Growth Dev. 2020;28(2):221-7. https://doi.org/10.34284/KJGD.2020.05.28.2.221
- 22. Lee HJ. Effects of the Tuina program on nurses with low back pain [dissertation]. Seoul: Hanyang University; 2002.
- 23. Hegewald J, Berge W, Heinrich P, Staudte R, Freiberg A, Scharfe J, et al. Do technical aids for patient handling prevent musculoskeletal complaints in health care workers?: a systematic review of intervention studies. Int J Environ Res Public Health. 2018;15(3):https://doi.org/10.3390/ijerph15030476
- 24. Kim SC, Kim SG, Kim CS. Effect of abdominal draw in maneuver in sitting position. J Rehabil Welfare Eng Assist Technol. 2017;11(3):207-14. https://doi.org/10.21288/resko.2017.11.3.207
- 25. Ahn JH, Kim HS, Kim HJ. Pain, disability, emotional status and educational needs between acute and chronic low back pain groups. J Korean Biol Nurs Sci. 2019;21(1):77-84. https://doi.org/10.7586/jkbns.2019.21.1.77
- 26. Chang IS, Kang HS. The effect of exercise for the prevention of low back pain on back pain, back strength, flexibility operating room nurses. J Korean Clin Nurs Res. 2004;10(1):125-33.
- 27. Lee K, Jung H. The effect of core program on back pain, back strength and flexibility to nurses. J Korean Data Anal Soc. 2007;9(4):1693-706.
- 28. Gill K, Krag MH, Johnson GB, Haugh LD, Pope MH. Repeatability of four clinical methods for assessment of lumbar spinal motion. Spine (Phila Pa 1976). 1988;13(1):50-3. https://doi.org/10.1097/00007632-198801000-00012
- 29. Abdollahi T, Pedram Razi S, Pahlevan D, Yekaninejad MS, Amaniyan S, Leibold Sieloff C, et al. Effect of an ergonomics educational program on musculoskeletal disorders in nursing staff working in the operating room: a quasi-randomized controlled clinical trial. Int J Environ Res Public Health. 2020;17(19):7333. https://doi.org/10.3390/ijerph17197333
- 30. Kim J, Lee JA, Choi SH, Hwang SS, Jung MH. Nurses and low back pain: a literature review. J Korean Soc Living Environ Syst. 2007;14(4):298-312.
- 31. Sung MH, Seo DH, Eum OB. Factors affecting low back pain in nurses in intensive care unit. J Korean Acad Fundam Nurs. 2010;17(3):343-50.
- 32. Sun W, Zhang H, Tang L, He Y, Tian S. The factors of non-specific chronic low back pain in nurses: a meta-analysis. J Back Musculoskelet Rehabil. 2021;34(3):343-53. https://doi.org/10.3233/BMR-200161