1Hanwha Techwin R&D Center, Seongnam
2College of Nursing, Hanyang University, Seoul, Korea
Copyright © 2016 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Variables | MetS (Current) | Non-MetS (Current) | x2 | p |
|---|---|---|---|---|
|
MetS (4 yrs ago) Non-MetS (4 yrs ago) |
Group 4: n=257, 6.6% Group 3: n=482, 12.4% |
Group 2: n=399, 10.3% Group 1: n=2,754, 70.8% |
209.07 | <.001 |

Comparison Male Workers' Characteristics by of Occupational Type (N=3,892)
| Variables | Office workers (n=774) | Non-Office workers (n=2,568) | Drivers (n=550) | x2 or F | p |
|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | |||
| Age (year) | 42.7±7.3a | 41.1±9.1b | 53.1±7.2c | 456.03 | <.001 |
| b<a<c | |||||
| Body Mass Index | 24.4±2.8a | 23.9±3.2b | 24.7.8±3.0c | 18.66 | <.001 |
| a=c>b | |||||
| Systolic blood pressure | 118.5±11.7a | 120.7±12.5b | 124.1±12.9c | 33.20 | <.001 |
| a<b<c | |||||
| Diastolic blood pressure | 73.8±9.1a | 76.4±9.2b | 76.9±9.7c | 27.85 | <.001 |
| a<b=c | |||||
| Fasting blood glucose | 96.2±14.9a | 100.9±24.6b | 101.3±33.1c | 12.01 | <.001 |
| a<b=c | |||||
| HDL cholesterol | 50.6±11.6a | 50.3±12.2b | 44.3±10.7c | 60.83 | <.001 |
| c<a=b | |||||
| Triglyceride | 144.6±87.7a | 158.9±101.8b | 202.1±107.7c | 57.06 | <.001 |
| a<b<c | |||||
| LDL cholesterol | 121.8±28.3a | 117.3±31.8b | 116.9±33.7c | 6.67 | .001 |
| a>b=c | |||||
| No. of MetS Risk Factors | 1.2±1.2a | 1.4±1.1b | 1.9±1.2c | 72.63 | <.001 |
| a<b<c | |||||
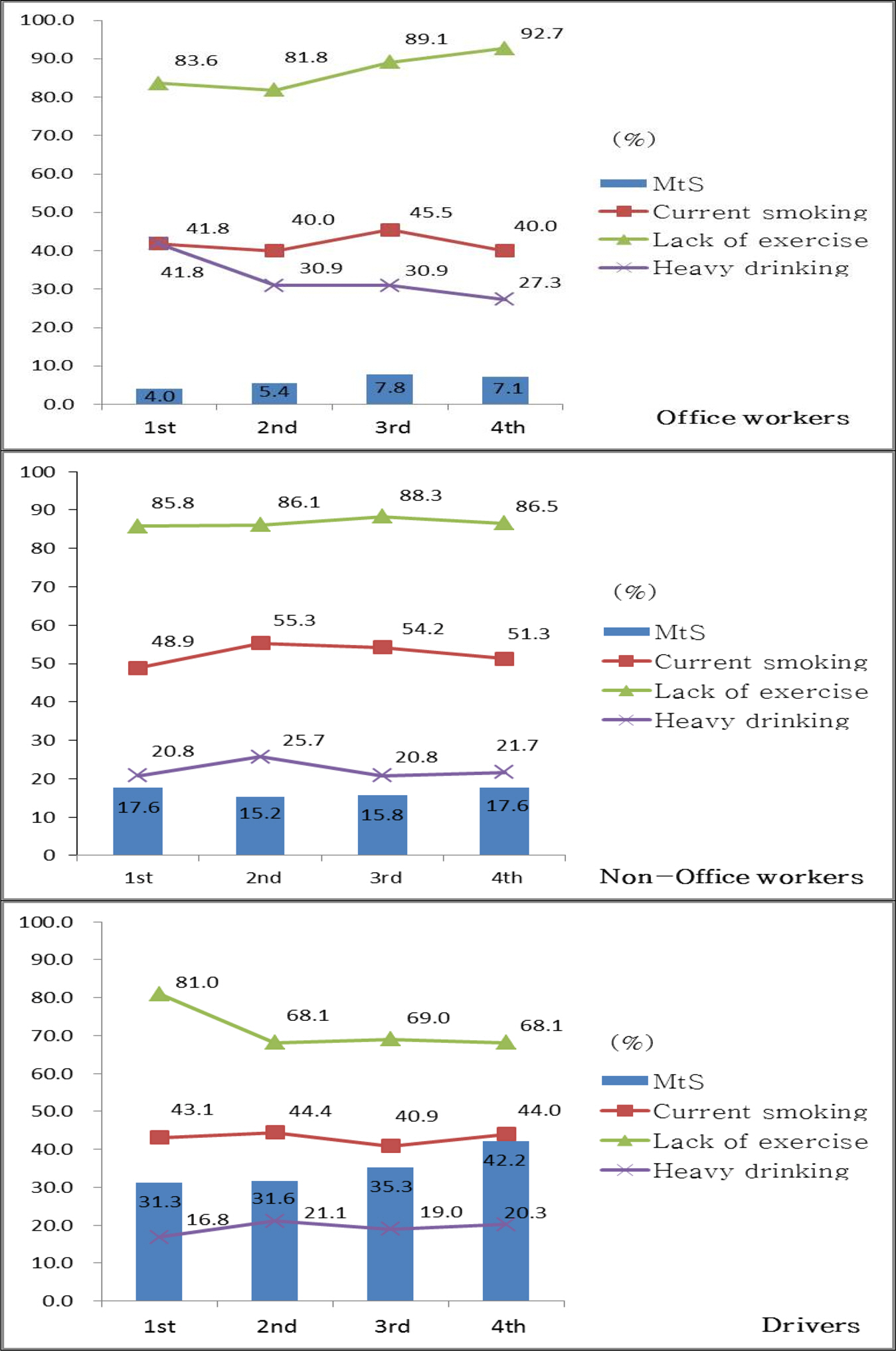
| Current smoking | 259 (33.5) | 1,261 (49.1) | 220 (40.0) | 64.61 | <.001 |
| Heavy drinking | 249 (32.2) | 523 (20.4) | 97 (17.6) | 55.92 | <.001 |
| Lack of exercise | 654 (84.5) | 2,175 (84.7) | 345 (62.7) | 150.88 | <.001 |
| Prevalence of 1st year | 31 (4.0) | 453 (17.6) | 172 (31.3) | 173.91 | <.001 |
| MetS 2nd year | 42 (5.4) | 391 (15.2) | 174 (31.6) | 168.58 | <.001 |
| 3rd year | 60 (7.8) | 406 (15.8) | 194 (35.3) | 179.99 | <.001 |
| 4th year | 55 (7.1) | 452 (17.6) | 232 (42.2) | 266.60 | <.001 |
HDL=high density lipoprotein; LDL=low density lipoprotein; MetS=Metabolic syndrome.
Prevalence of Metabolic Syndrome Current and Four Years ago (N=3,892)
| Variables | MetS (Current) | Non-MetS (Current) | x2 | p |
|---|---|---|---|---|
| MetS (4 yrs ago) Non-MetS (4 yrs ago) |
Group 4: n=257, 6.6% Group 3: n=482, 12.4% |
Group 2: n=399, 10.3% Group 1: n=2,754, 70.8% |
209.07 | <.001 |
MetS=Metabolic syndrome; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).
Differences in Male Workers' Characteristics of Four Sub-groups (N=3,892)
| Variables | Group 1 (n=2,754) | Group 2 (n=399) | Group 3 (n=482) | Group 4 (n=257) | x2 or F (p) | Scheffé |
|---|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | |||
| Age(year) | 41.9±9.0a | 45.3±10.3b | 45.2±9.4c | 49.1±9.3d | 68.76 (<.001) | a<b=c<d |
| Body mass index | 23.5±2.8a | 24.2±3.0b | 26.2±3.1c | 26.9±3.4d | 194.23 (<.001) | a<b<c<d |
| Occupation | 388.49 (<.001) | |||||
| Non-Office workers | 1,807 (70.4) | 309 (12.0) | 308 (12.0) | 144 (5.6) | ||
| Office workers | 700 (90.4) | 19 (2.5) | 43 (5.6) | 12 (1.6) | ||
| Drivers | 247 (44.9) | 71 (12.9) | 131 (23.8) | 101 (18.4) | ||
| Total cholesterol | 197.5±34.7a | 202.0±35.5b | 208.5±39.0c | 206.1±38.5d | 16.38 (<.001) | a<c=d |
| HDL cholesterol | 51.6±11.7a | 50.8±12.3b | 41.3±9.1c | 40.3±9.7d | 172.67 (<.001) | a=b>c=d |
| Triglyceride | 136.9±80.2a | 151.7±88.4b | 264.5±122.5c | 256.7±106.2d | 383.06 (<.001) | a=b<c=d |
| LDL cholesterol | 118.8±30.7a | 120.7±31.0b | 114.9±34.2c | 114.0±33.5d | 4.47 (.004) | b>c=d |
| Current smoking | 1,194 (43.4) | 190 (47.6) | 229 (47.5) | 127 (49.4) | 7.24 (.065) | |
| Heavy drinking | 629 (22.8) | 80 (20.1) | 102 (21.2) | 58 (22.6) | 2.00 (.573) | |
| Lack of exercise | 2,263 (82.2) | 311 (77.9) | 392 (81.3) | 208 (80.9) | 4.23 (.237) |
HDL=high density lipoprotein; LDL=low density lipoprotein; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).
Predicting Factors on the Current Prevalence of MetS Compared with Non-MetS
| Variables | Group 3 (n=482) vs Group 1 (n=2,754) | Group 4 (n=257) vs Group 2 (n=399) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | Exp (B) | 95% CI | p | B | SE | Exp (B) | 95% CI | p | ||
| Age (year) | 0.02 | .01 | 1.02 | 1.01~1.04 | <.001 | 0.02 | .01 | 1.02 | 1.00~1.04 | .026 | |
| Current smoking | 0.17 | .10 | 1.18 | 0.96~1.45 | .112 | 0.17 | .17 | 1.18 | 0.73~1.43 | .335 | |
| Lack of exercise (<<3 times/week) | 0.26 | .14 | 1.29 | 0.98~1.68 | .061 | 0.44 | .21 | 1.55 | 1.02~2.35 | .041 | |
| Heavy drinking (≥≥3 times/week) | 0.29 | .10 | 1.34 | 1.09~1.64 | .005 | 0.02 | .17 | 1.02 | 0.73~1.43 | .903 | |
| Occupation type | Non-office workers | 1.09 | .17 | 2.99 | 2.13~4.18 | <.001 | -0.18 | .39 | 0.84 | 0.39~1.81 | .646 |
| Drivers | 2.08 | .21 | 7.97 | 4.89~10.83 | <.001 | 0.79 | .42 | 2.21 | 1.03~2.94 | .050 | |
MetS=Metabolic syndrome; Reference groups: Non- or Ex-smoking, exercise≥3 times/week, alcohol drinking<3 times/week, Office workers; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).
HDL=high density lipoprotein; LDL=low density lipoprotein; MetS=Metabolic syndrome.
MetS=Metabolic syndrome; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).
HDL=high density lipoprotein; LDL=low density lipoprotein; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).
MetS=Metabolic syndrome; Reference groups: Non- or Ex-smoking, exercise≥3 times/week, alcohol drinking<3 times/week, Office workers; Group 1 (Non-MetS → Non-MetS); Group 2 (MetS → Non-MetS); Group 3 (Non-MetS → MetS); Group 4 (MetS → MetS).