1College of Nursing, Keimyung University ․ Research Institute of Nursing Science, Keimyung University, Daegu
2Graduate School, Keimyung University, Daegu
3Department of Nursing, Hosan University, Gyeongsan, Korea
Copyright © 2016 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.

ADL=activity of daily living; BPC=behavioral problems checklist; DBS=disruptive behavior scale; CMAI=cohen-mansfield agitation inventory; RMBPC=revised memory and behavior problem checklist; BEHAVE-AD=behavioral pathology in Alzheimer's disease scale; NPI=neuropsychiatric inventory; PGDRS=psychogeriatric dependency rating scale; BSRS=behavior symptom rating scale; NPI-NH=neuropsychiatric inventory nursing home version; MDS=minimum data set.
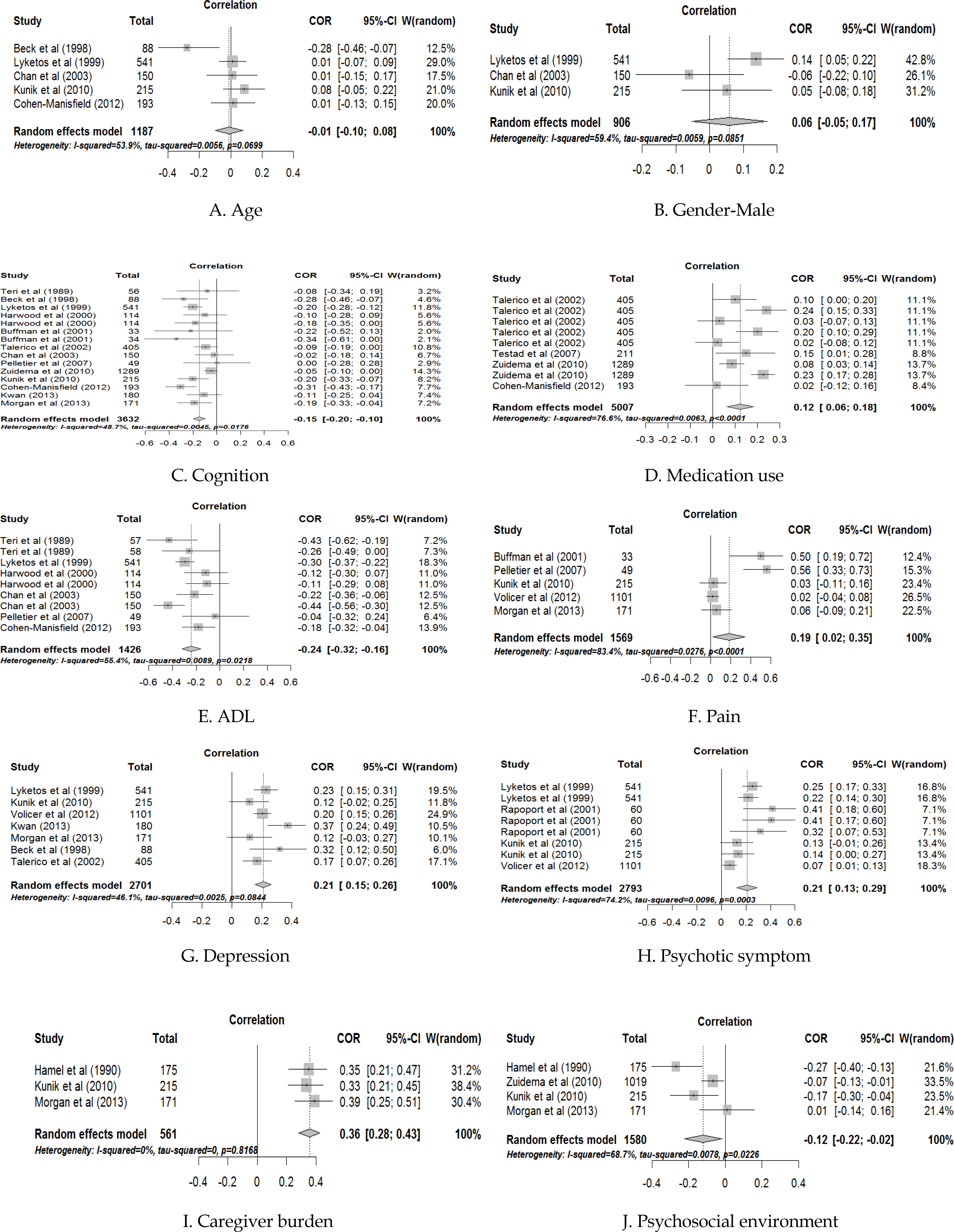
| Variables | Categories | k | ES | -95% CI | +95% CI | I2 (%) | Qb (p) | R2 (%) |
|---|---|---|---|---|---|---|---|---|
| Setting | Community & outpatient clinic | 7 | -.17 | -.22 | -.11 | 0.0 | 0.07 | |
| Nursing home & long-term facility | 8 | -.15 | -.24 | -.07 | 61.4 | (.789) | ||
| Severity of dementia | Below & moderate | 8 | -.14 | -.20 | -.09 | 5.4 | 0.19 | |
| Severe | 7 | -.16 | -.25 | -.07 | 68.6 | (.662) | ||
| Cognition measurement | Type of score | 13 | -.17 | -.22 | -.12 | 18.3 | 11.10 | 80.7 |
| Type of grade | 2 | -.05 | -.10 | -.01 | 0.0 | (<.001) | ||
| Agitation measurement | CMAI | 6 | -.20 | -.25 | -.14 | 0.0 | 2.39 | |
| Others | 9 | -.13 | -.19 | -.06 | 52.6 | (.122) |
k=number of studies; CI=confidence interval; I
2=the proportion of true variance; Qb=value between subgroup; R
2=the proportion of explained between study variance; MMSE=mini-mental state examination; DRS=dementia rating scale; FAST=functional assessment staging; GDS=global deterioration scale; CMAI=cohen-mansfield agitation inventory.

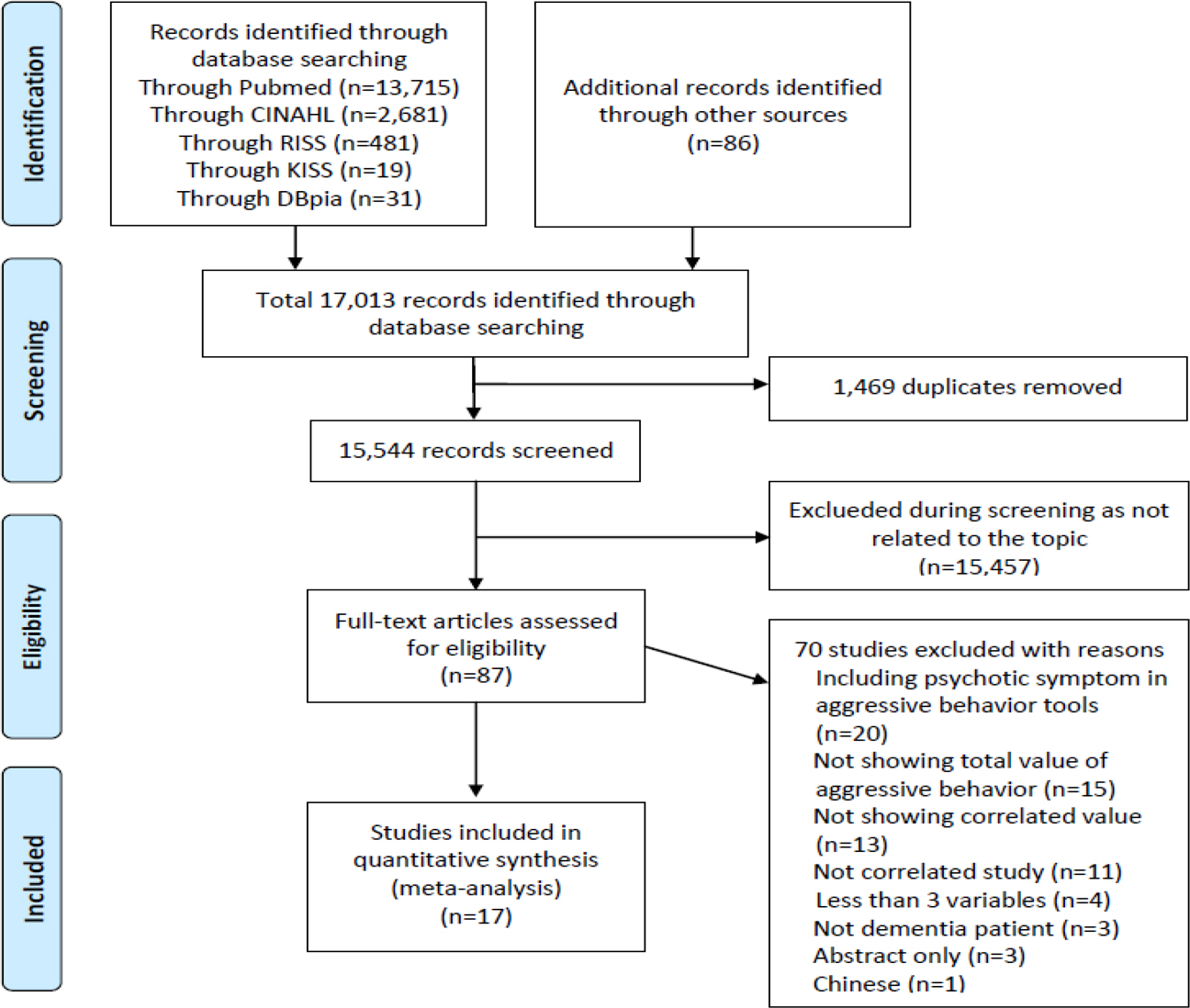
Characteristics of Studies Included in Meta-Analysis
| Researchers (year) | Country | Publication | Sample size | e Setting | Related variables | Agitation measurement | Quality assessment |
|---|---|---|---|---|---|---|---|
| Teri et al. (1989)a1) | USA | Journal | 56 | Community | Cognition, ADL | BPC | 10 |
| Hamel et al. (1990)a2) | Canada | Journal | 175 | Community | Caregiver burden, | Ryden aggression scale | 10 |
| Psychosocial environment | |||||||
| Beck et al. (1998)a3) | USA | Journal | 88 | Nursing home | Age, Cognition, | DBS | 11 |
| Depression | |||||||
| Lyketsos et al. (1999)a4) | USA | Journal | 541 | Community | Age, Gender, Cognition, | CMAI | 10 |
| ADL, Depression, | |||||||
| Psychotic symptom | |||||||
| Harwood et al. (2000)a5) | USA | Journal | 114 | Outpatient clinic | Cognition, ADL | RMBPC, BEHAVE-AD | 9 |
| Buffum et al. (2001)a6) | USA | Journal | 33 | Nursing home | Cognition, Pain | CMAI | 10 |
| Rapoport et al. (2001)a7) | Canada | Journal | 60 | Outpatient clinic | Psychotic symptom | NPI-agitation | 9 |
| Talerico et al. (2002)a8) | USA | Journal | 405 | Nursing home | Cognition, Medication use, | PGDRS | 10 |
| Depression | |||||||
| Chan et al. (2003)a9) | USA | Journal | 150 | Community | Age, Gender, Cognition, | BSRS | 9 |
| ADL | |||||||
| Pelletier et al. (2007)a10) | Canada | Journal | 49 | Long-term facility | Cognition, ADL, Pain | CMAI | 11 |
| Testad et al. (2007)a11) | Norway | Journal | 211 | Nursing home | Medication use | CMAI | 9 |
| Zuidema et al. (2010)a12) | Netherlands | s Journal | 1019 | Nursing home | Cognition, Medication use, | NPI-NH agitation *disinhibition *irritability | 11 |
| Psychosocial environment | |||||||
| Kunik et al. (2010)a13) | USA | Journal | 215 | Community | Age, Gender, Cognition, | CMAI | 11 |
| Pain, Depression, | |||||||
| Psychotic symptom, | |||||||
| Caregiver burden, | |||||||
| Psychosocial environment | |||||||
| Volicer et al. (2012)a14) | Netherlands | s Journal | 1101 | Nursing home | Pain, Depression, | MDS | 10 |
| Psychotic symptom | |||||||
| Cohen-Mansfield et al. (2012)a15) | d USA | Journal | 193 | Nursing home | Age, Cognition, | Agitation Behavior Mapping Inventory | 10 |
| Medication use, ADL | |||||||
| Kwan (2013)a16) | Korea | Thesis | 180 | Nursing home | Cognition, Depression | Ryden aggression scale | 10 |
| Morgan et al. (2013)a17) | USA | Journal | 171 | Community | Cognition, Pain, Depression | , CMAI | 11 |
| Caregiver burden, | |||||||
| Psychosocial environment |
ADL=activity of daily living; BPC=behavioral problems checklist; DBS=disruptive behavior scale; CMAI=cohen-mansfield agitation inventory; RMBPC=revised memory and behavior problem checklist; BEHAVE-AD=behavioral pathology in Alzheimer's disease scale; NPI=neuropsychiatric inventory; PGDRS=psychogeriatric dependency rating scale; BSRS=behavior symptom rating scale; NPI-NH=neuropsychiatric inventory nursing home version; MDS=minimum data set.
Subgroup Analysis of Moderator Variables in Cognition
| Variables | Categories | k | ES | -95% CI | +95% CI | I |
Qb (p) | R |
|---|---|---|---|---|---|---|---|---|
| Setting | Community & outpatient clinic | 7 | -.17 | -.22 | -.11 | 0.0 | 0.07 | |
| Nursing home & long-term facility | 8 | -.15 | -.24 | -.07 | 61.4 | (.789) | ||
| Severity of dementia | Below & moderate | 8 | -.14 | -.20 | -.09 | 5.4 | 0.19 | |
| Severe | 7 | -.16 | -.25 | -.07 | 68.6 | (.662) | ||
| Cognition measurement | Type of score | 13 | -.17 | -.22 | -.12 | 18.3 | 11.10 | 80.7 |
| Type of grade | 2 | -.05 | -.10 | -.01 | 0.0 | (<.001) | ||
| Agitation measurement | CMAI | 6 | -.20 | -.25 | -.14 | 0.0 | 2.39 | |
| Others | 9 | -.13 | -.19 | -.06 | 52.6 | (.122) |
k=number of studies; CI=confidence interval; I
2=the proportion of true variance; Qb=value between subgroup; R
2=the proportion of explained between study variance; MMSE=mini-mental state examination; DRS=dementia rating scale; FAST=functional assessment staging; GDS=global deterioration scale; CMAI=cohen-mansfield agitation inventory.
ADL=activity of daily living; BPC=behavioral problems checklist; DBS=disruptive behavior scale; CMAI=cohen-mansfield agitation inventory; RMBPC=revised memory and behavior problem checklist; BEHAVE-AD=behavioral pathology in Alzheimer's disease scale; NPI=neuropsychiatric inventory; PGDRS=psychogeriatric dependency rating scale; BSRS=behavior symptom rating scale; NPI-NH=neuropsychiatric inventory nursing home version; MDS=minimum data set.
k=number of studies; CI=confidence interval; I =the proportion of true variance; Qb=value between subgroup; R =the proportion of explained between study variance; MMSE=mini-mental state examination; DRS=dementia rating scale; FAST=functional assessment staging; GDS=global deterioration scale; CMAI=cohen-mansfield agitation inventory.