1Chonnam Research Institute of Nursing Science, Gwangju, Korea
2Department of Nursing, Kwangju Women's University, Gwangju, Korea
3College of Nursing, Chonnam National University, Gwangju, Korea
© 2018 Korean Society of Adult Nursing
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/ by-nc/3.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Variables | Stigma | Self-blame | Distress |
|---|---|---|---|
| r (p) | r (p) | r (p) | |
| Stigma | 1 | .59 (<.001) | .37 (<.001) |
| Self-blame | 1 | .45 (<.001) | |
| Distress | 1 |

Stigma, Self-blame, and Distress according to General Characteristics of Participants (N=247)
| Variables | Categories | n (%) or M±SD | Stigma | Self-blame | Distress | |||
|---|---|---|---|---|---|---|---|---|
| M± SD | t or F (p) | M± SD | t or F (p) | M± SD | t or F (p) | |||
| Age (year) | 40~49 | 72(29.3) | 36.49±9.00 | 1.23 | 20.57±7.96 | 2.11 | 9.63±6.43 | 1.30 |
| 50~59 | 60(24.4) | 35.42±9.70 | (.300) | 19.63±7.77 | (.100) | 7.68±7.42 | (.275) | |
| 60~69 | 68(27.6) | 35.60±8.40 | 17.51±6.28 | 7.68±7.00 | ||||
| ≥70 | 46(18.7) | 33.24±9.22 | 19.22±7.15 | 7.83±6.77 | ||||
| 57.3±12.3 | 35.37±9.07 | 19.24±7.38 | 8.28±6.91 | |||||
| Gender | Men | 98(39.7) | 36.11±9.26 | 1.08 | 18.48±6.84 | -1.34 | 6.06±5.88 | -4.20 |
| Women | 149(60.3) | 34.84±8.93 | (.281) | 19.76±7.66 | (.182) | 9.71±7.16 | (<.001) | |
| Spouse | Yes | 215(87.0) | 34.90±8.81 | -1.99 | 18.99±7.37 | -1.44 | 8.05±6.69 | -1.28 |
| No | 32(13.0) | 38.31±10.27 | (.047) | 21.00±7.17 | (.150) | 9.72±8.17 | (.202) | |
| Religion | None | 85(34.4) | 34.39±8.22 | 1.14 | 18.19±6.98 | 0.85 | 8.27±6.86 | 0.52 |
| Protestantism | 75(30.4) | 36.32±10.29 | (.336) | 19.96±7.64 | (.496) | 7.53±6.48 | (.723) | |
| Catholicism | 24(9.7) | 37.63±9.06 | 19.83±8.00 | 8.96±7.26 | ||||
| Buddhism | 60(24.3) | 34.83±8.58 | 19.78±7.39 | 9.00±7.40 | ||||
| Others | 3(1.2) | 30.00±6.56 | 16.33±4.93 | 6.00±7.94 | ||||
| Monthly household income (10,000 won) | 50~<100 | 97(39.3) | 34.15±8.34 | 1.06 | 19.14±7.30 | 1.28 | 7.41±7.38 | 0.85 |
| 100~<200 | 93(37.7) | 35.84±9.88 | (.369) | 18.49±7.33 | (.281) | 8.69±6.72 | (.466) | |
| 200~<300 | 32(13.0) | 36.84±10.14 | 21.19±6.85 | 9.31±6.95 | ||||
| ≥300 | 25(10.0) | 36.48±6.91 | 20.48±8.46 | 8.48±5.65 | ||||
| Education level | Illiteracy | 15(6.0) | 34.93±11.76 | 1.71 | 21.60±7.78 | 2.20 | 9.80±9.69 | 2.10 |
| Elementary | 47(19.0) | 32.77±6.39 | (.149) | 17.28±5.66 | (.069) | 6.51±6.16 | (.081) | |
| Middle school | 58(23.5) | 34.69±8.47 | 18.21±6.58 | 7.38±7.05 | ||||
| High school | 91(36.8) | 36.63±10.14 | 19.88±7.90 | 8.66±6.67 | ||||
| ≥ College | 36(14.7) | 36.69±8.44 | 20.94±8.39 | 10.33±6.40 | ||||
| Cancer stage | I | 58(23.5) | 33.45±7.67 | 1.19 | 18.03±7.15 | 8.79 | 8.91±7.19 | 1.69 |
| II | 41(16.6) | 36.22±8.70 | (.310) | 20.29±6.46 | (.452) | 10.05±7.34 | (.170) | |
| III | 47(19.0) | 35.36±10.54 | 19.11±7.72 | 7.38±6.29 | ||||
| IV | 101(40.9) | 36.07±9.18 | 19.59±7.66 | 7.57±6.76 | ||||
| Diagnosis | Colon cancer a | 50(20.3) | 38.20±11.30 | 1.96 | 20.06±7.56 | 2.50 | 8.80±5.48 | 8.70 |
| Breast cancer b | 51(20.6) | 33.94±7.71 | (.101) | 18.73±7.86 | (.044) | 8.53±6.44 | (.001) | |
| Cervix cancer c | 50(20.3) | 35.55±9.16 | 21.30±7.14 | 12.34±7.73 | c> d, e | |||
| Gastric cancer d | 49(19.8) | 35.28±8.40 | 16.90±6.53 | 5.90±5.96 | ||||
| Lung cancer e | 47(19.0) | 33.76±8.00 | 19.23±7.19 | 5.53±6.72 | ||||
Descriptive Statistics of Research Variables (N=247)
| Variables | M± SD | Item number (scoring) | Range | Mean/item± SD | |
|---|---|---|---|---|---|
| Possible | Actual | ||||
| Stigma | 35.34±9.07 | 24 (1~4) | 24~96 | 24~86 | 1.41±0.36 |
| Self-blame | 19.25±7.36 | 10 (1~5) | 10~50 | 10~46 | 1.93±0.74 |
| Distress | 8.26±6.90 | 3 (0~10) | 0~30 | 0~30 | 2.75±2.30 |
Relationships between Stigma, Self-blame, and Distress (N=247)
| Variables | Stigma | Self-blame | Distress |
|---|---|---|---|
| r (p) | r (p) | r (p) | |
| Stigma | 1 | .59 (<.001) | .37 (<.001) |
| Self-blame | 1 | .45 (<.001) | |
| Distress | 1 |
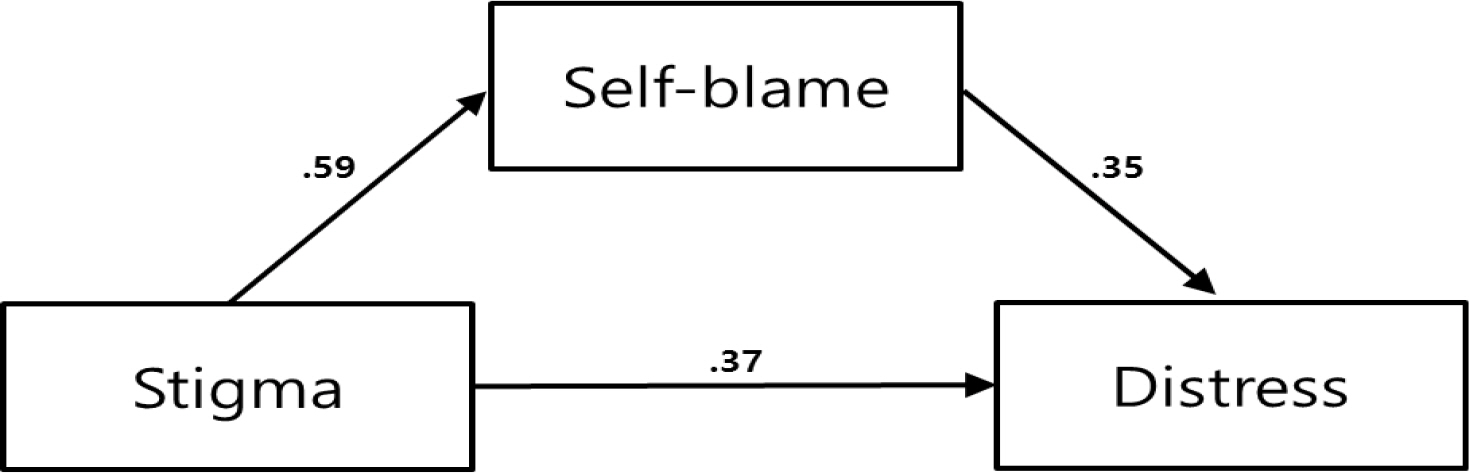
Mediating Effect of Self-blame in the Relationships between Stigma and Distress (N=247)
| Step | Variables | B | β | t | p | Adj. R2 | F | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Stigma | → | Self-blame | .48 | .59 | 11.39 | <.001 | .343 | 129.66 | <.001 |
| Step 2 | Stigma | → | Distress | .49 | .37 | 6.14 | <.001 | .130 | 37.64 | <.001 |
| Step 3 | Stigma, Self-blame | → | Distress | .209 | 33.48 | <.001 | ||||
| 1) Stigma | → | Distress | .21 | .16 | 2.23 | .027 | ||||
| 2) Self-blame | → | Distress | .59 | .35 | 5.06 | <.001 | ||||
| Sobel test : Z=3.64, p<.001 | ||||||||||