Abstract
-
Purpose
This study developed a self-management program for patients undergoing lumbar spinal stenosis surgery utilizing the information-motivation-behavioral skills (IMB) model.
-
Methods
This study employed a quasi-experimental design with a nonequivalent control group and pretest–posttest design. Data were collected from August 11, 2022, to March 31, 2023, at a general hospital in South Korea. A total of 58 patients participated in the study (30 experimental, 28 control group). The experimental group received a six-session self-management program based on the IBM model, whereas the control group received usual education and information. Data were analyzed with SPSS/WIN 23.0 using the independent t-test, chi-square test, Fisher’s exact test, Shapiro-Wilk test, and Mann-Whitney U test.
-
Results
Significant differences were observed in self-management information (p<.001), personal motivation (p=.002), social motivation (p=.002), behavioral skills (p=.002), behaviors (p=.003), health-related quality of life (p<.001), and disc height (p=.006) in the experimental group following program implementation, compared to the control group. However, no significant differences were found in lower extremity muscular strength, lumbar lordotic angle, or the visual analog scores for low back pain and leg pain between the two groups.
-
Conclusion
The self-management program developed in this study, based on the IMB model, was effective in improving self-management information, motivation, behavioral skills, behaviors, health-related quality of life, and self-management health outcomes in patients undergoing lumbar spinal stenosis surgery. Nevertheless, future research should aim to verify the long-term effects of such self-management programs by extending the intervention period.
-
Key Words: Spinal stenosis; Self-management; Information motivation behavioral skills model; Health-related quality of life
INTRODUCTION
Lumbar spinal stenosis surgery is the second most frequently performed spinal surgery in South Korea, with the number of patients increasing by 30% over the past 5 years [
1]. As the population continues to age, this trend is expected to accelerate, highlighting the importance of prevention and ongoing management. Therefore, ongoing postoperative self-management is essential for maintaining spinal health.
The treatment for lumbar spinal stenosis includes a range of approaches, from conservative therapies such as medication, physical therapy, and injections to surgical intervention. Posterior lumbar fusion surgery is recognized as an effective option; however, postoperative complications such as pain recurrence and diminished physical function remain possible [
2]. Previous research has indicated that 14% of patients require reoperation within 5 years [
3], leading to physical and psychological challenges as well as decreased quality of life [
4]. Furthermore, after a certain period post-surgery, disc height and lumbar lordosis may decline due to weight-bearing forces [
5], potentially resulting in issues such as reduced lower limb strength and impaired gait [
6].
Patients undergoing lumbar spinal stenosis surgery often need substantial time to recover functional abilities and reintegrate into daily life [
7]. This underscores the critical importance of postoperative patient education and effective self-management. While surgical intervention typically alleviates physical burdens, pain, and gait disturbances [
8], sustaining long-term health without continued self-management remains a challenge. Currently, hospitals tend to offer only medication and basic care education [
9], and structured self-management education programs to support post-discharge health maintenance are lacking. Therefore, the development of self-management programs is vital to empower patients to actively manage their spinal health and adopt health-promoting behaviors.
The effectiveness of such a program was evaluated using clinical indicators relevant to patients after lumbar spinal stenosis surgery, including lower limb strength, pain levels, intervertebral disc height, and lumbar lordosis. These variables were chosen because they represent primary postoperative concerns, such as pain recurrence, reduced mobility, and structural changes in the spine, which, if unaddressed, can negatively affect recovery and long-term quality of life. Thus, these outcomes served as meaningful metrics for assessing the practical impact of the self-management program.
The present study aimed to develop and evaluate a self-management program for patients undergoing lumbar spinal stenosis surgery, grounded in the information-motivation-behavioral skills (IMB) model [
10]. The IMB model posits that health behavior change is achieved through information provision, motivation enhancement, and the improvement of behavioral skills, ultimately promoting healthy behaviors. This model has demonstrated effectiveness in encouraging self-management across a range of chronic conditions, including type 1 diabetes, hypertension, heart failure, coronary artery disease, chronic obstructive pulmonary disease, inflammatory bowel disease, and knee osteoarthritis [
11]. It suggests that health behaviors are influenced by the interplay of information, motivation, and behavioral skills. Nevertheless, most existing studies have focused on exercise interventions, and few have applied the IMB model to self-management education specifically for patients undergoing lumbar spinal stenosis surgery.
Accordingly, this study aimed to apply the IMB model within a self-management program to improve patients’ disease-related knowledge, motivation, and behavioral skills, with the goal of enhancing self-management practices and quality of life. The program was systematically structured based on the IMB model and designed to help patients sustain long-term health-promoting behaviors.
Program effectiveness was evaluated by examining improvements in lower limb strength, pain reduction, and the maintenance of disc height and lumbar lordosis—outcomes that are clinically relevant after lumbar spinal stenosis surgery. Decreases in disc height, reduced lumbar lordosis, lower limb weakness, and recurrent pain may result in secondary problems if not managed appropriately. Therefore, these indicators were regarded as key measures of program effectiveness. By addressing the current gap in postoperative self-management education for patients with lumbar spinal stenosis, this study aimed to promote improved long-term health and quality of life.
METHODS
1. Study Design
This study employed a quasi-experimental design utilizing a non-equivalent control group and a non-synchronized design.
2. Setting and Samples
The target population of this study was patients diagnosed with lumbar spinal stenosis who underwent their first laminectomy and posterior lumbar fusion surgery at a general hospital in South Korea. The inclusion criteria were: (1) adults aged 19 years or older with the ability to communicate, (2) no history of previous spinal surgery, (3) diagnosis of lumbar spinal stenosis, (4) scheduled for laminectomy and posterior lumbar fusion surgery for the first time, and (5) ability to read and understand Korean and willingness to provide informed consent. The exclusion criteria were patients with (1) other neurological or musculoskeletal disorders that could affect functional outcomes, (2) cognitive impairment or psychiatric illness that could interfere with participation, or (3) refusal to participate in the study.
The required sample size was calculated using G*Power 3.1.9.4 software. According to a previous study [
12], an independent t-test required a sample size based on an effect size of 0.80, a significance level (α) of 0.05, and a power (1–β) of 0.80, yielding a total sample size of 52 participants (26 per group). Considering a potential dropout rate of 20%, 30 participants were recruited for each group. Participants were assigned to the experimental or control group according to the order of admission to the hospital, without randomization. However, two participants from the control group declined to participate, resulting in a final sample of 30 participants in the experimental group and 28 in the control group (total: 58 participants).
This study was reported in accordance with the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) guidelines.
3. Measurements
The self-management knowledge measurement tool 1) self-management knowledge, 2) personal motivation for self-management, 3) social motivation for self-management, 4) self-management behavioral skills, 5) health-related quality of life (HRQoL), 6) lower limb strength, 7) lower back pain, 8) intervertebral disc height, 9) the lumbar lordosis angle used in this study was adapted from the disease-related knowledge assessment developed by Jeong and Lee [
13] for patients undergoing spinal surgery. This tool consists of 14 items addressing brace management (two items), medication and treatment (three items), daily activities (six items), harmful lifestyle habits (two items), and exercise management (three items). Each item was scored as “yes” (1 point) or “no/don’t know” (0 points), with higher scores reflecting greater self-management knowledge. The reliability of this tool was shown by a Cronbach’s α value of .91 in Jeong and Lee’s study [
13] and a Kuder–Richardson Formula 20 (KR-20) value of .60 in this study.
Personal motivation for self-management was assessed using the Health Attitude Scale developed by Torabi et al. [
14] and translated into Korean by Kim [
15]. This instrument comprises 15 items categorized into health-related emotions (five items), beliefs about disease prevention and healthy lifestyles (five items), and intention to practice healthier behaviors (five items). Each item was rated on a 5-point Likert scale (1=strongly disagree to 5=strongly agree), with higher scores indicating stronger personal motivation. Reliability was shown by Cronbach’s α values of .88 in Kim’s study [
15] and .84 in this study.
Social motivation for self-management was measured using the Social Support Scale developed by Zimet et al. [
16] and translated into Korean by Shin and Lee [
17]. This instrument includes 12 items covering family support (four items), peer support (four items), and medical staff support (four items), each rated on a 5-point Likert scale (1=strongly disagree to 5=strongly agree). Higher scores indicate greater social motivation. The reliability was shown by Cronbach’s α values of .88 in Shin and Lee’s study [
17] and .87 in this study.
Self-management behavioral skills were measured using the Self-Efficacy Scale developed by Marcus et al. [
18] and translated into Korean by Lee and Chang [
19]. This scale contains five items scored on a 5-point Likert scale (1=not confident at all to 5=very confident), with higher scores indicating stronger self-management behavioral skills. The reliability was demonstrated by Cronbach’s α values of .82 in Lee and Chang’s study [
19] and .88 in this study.
Self-management behaviors were measured using the Self-Management Behavior Assessment tool developed by Jeong and Lee [
13]. This tool comprises 14 items covering brace management (two items), medication and treatment (three items), daily activities (six items), harmful lifestyle habits (two items), and exercise management (three items). Each item was rated on a 5-point Likert scale (1=never to 5=always), with higher scores reflecting greater engagement in self-management behaviors. The tool’s reliability was shown by Cronbach’s α values of .95 in Jeong and Lee’s study [
13] and .88 in this study.
HRQoL was assessed using the Euro Quality of Life Questionnaire 5-Dimensional Classification (EQ-5D). This instrument includes five items: mobility, self-care, daily activities, pain/discomfort, and anxiety/depression, each rated on a 3-point Likert scale (1=no problems, 2=some problems, 3=severe problems). Final scores were calculated according to the weighting method described by Nam et al. [
20].
Lower limb strength was measured using the sit-to-stand-five-times test (STS5 test). Participants were instructed to sit on a chair with armrests, cross their arms over their chest, and stand up and sit down five times. The total time required was recorded, and the test was repeated twice to minimize measurement errors, with the average time used for analysis.
Lower back pain was assessed using the visual analog scale (VAS), in which participants marked their pain on a scale from 0 (no pain) to 10 (worst pain possible). Leg pain was evaluated using the same VAS methodology.
Intervertebral disc height was measured based on the Farfan Index [
21], which calculates the ratio of the total anterior and posterior disc height to disc diameter using lateral plain radiographs. Measurements were obtained via the picture archiving and communication system (PACS), and the procedure was repeated twice to reduce measurement error; the average value was used for analysis.
The lumbar lordosis angle was assessed using Cobb’s angle, determined by drawing lines across the upper endplates of the first and fifth lumbar vertebrae. Measurements were obtained using PACS, with the average of two measurements recorded to ensure accuracy.
4. Data Collection/Procedure
This study implemented a six-session individualized self-management program over a four-week period for patients undergoing lumbar spinal stenosis surgery. Given the nature of the surgery, the program was delivered one-on-one and encompassed six phases: pre-hospitalization, pre-surgery, surgery day, postoperative day 3, postoperative week 1, and postoperative week 3. Educational sessions were conducted face-to-face using self-management booklets, lumbar health checklists, and videos.
The study was conducted during the coronavirus disease 2019 pandemic; to comply with the Korea Disease Control and Prevention Agency’s social distancing guidelines, group education was excluded in favor of individualized education. To minimize the risk of respiratory infection, both researchers and participants wore Korea Filter 94 masks, used hand sanitizers, and followed strict personal hygiene protocols. A pilot study involving three patients scheduled for spinal surgery was conducted to assess the feasibility and applicability of the program.
A spinal center nurse served as a research assistant, supporting participant recruitment and obtaining informed consent. The primary researcher provided the research assistant with training in questionnaire administration and study protocols, ensuring familiarity with the intervention content prior to implementation. The program itself was delivered by the primary researcher, a registered nurse with over 15 years of clinical experience in an orthopedic ward. To maintain consistent and effective program delivery, the educator thoroughly reviewed key concepts related to the IMB model, adult learning theory, and patient-centered communication strategies during program development.
The primary objective of the program was to provide information, enhance motivation, and promote behavioral implementation, with the ultimate goal of improving patients’ self-management skills. The intervention emphasized tailored education, continuous feedback from healthcare providers, and social support to increase self-management success rates, optimize post-surgical recovery, and facilitate rehabilitation.
The first session took place prior to hospitalization during an outpatient visit, providing information about spinal disorders and surgical treatments to improve disease understanding. Personal motivation was fostered by setting self-management goals, and patients were encouraged to maintain a lumbar health journal and spinal health checklist. Hospital resources were introduced, and the researcher’s contact information was provided to ensure ongoing support. The session was individualized using educational booklets developed by the researcher.
The second session was conducted on the day of admission and included detailed education on preoperative and postoperative procedures, ensuring that patients fully understood the surgical process. Patients were encouraged to continue using their health journals and checklists, and the surgical transfer process was explained to help reduce preoperative anxiety. Social motivation was reinforced with videos showcasing successful self-management cases.
The third session took place on the day of surgery, focusing on postoperative education regarding proper posture, drain management, medication adherence, dietary management, and complication prevention. Patients received personalized education, and their adherence to self-management was assessed to increase their confidence in postoperative self-care. Ongoing medical support and feedback were provided to further strengthen social motivation.
The fourth session occurred on the third day after surgery, once patients could walk with spinal braces. Education was reiterated regarding postoperative management, including brace use, exercise, diet, and medication adherence. Progress toward individual goals was reviewed, and patients were encouraged to continue maintaining their health journals and checklists. Individualized consultations were provided to allow patients to discuss concerns and receive feedback from healthcare providers.
The fifth session was held one week after surgery, incorporating a true/false quiz to correct misconceptions and reinforce accurate health knowledge. Problem-solving strategies were introduced to improve patients’ coping abilities during recovery. Video testimonials of successful rehabilitation cases were provided to offer encouragement and promote family support. Feedback was given to improve self-efficacy and encourage sustained self-management.
The sixth session took place three weeks after surgery at the time of discharge. Comprehensive self-management education was delivered to ensure patients could continue proper care at home. Key topics such as regular exercise, correct posture, and independent daily care were reinforced through booklets and videos. Individual consultations addressed remaining concerns and provided further problem-solving strategies. Patients reviewed personal goals, received encouragement for social reintegration, and were provided with feedback to further support self-efficacy (
Table 1).
Patients in the control group received standard postoperative nursing care as provided by the hospital. This included preoperative consultations regarding treatment schedules and general postoperative nursing care, such as medication management and physical therapy guidance. This approach ensured that any observed effects could be attributed specifically to the IMB model–based self-management intervention.
5. IMB Model–Based Self-Management Program
In this study, the IMB model was applied to patients undergoing lumbar spinal stenosis surgery in recognition of the need for continuous self-management following discharge. The IMB model served as a theoretical framework for encouraging behavioral change by systematically delivering information, enhancing motivation, and developing behavioral skills tailored to this patient population. To inform program development, intervention programs and previous studies related to lumbar spinal stenosis were reviewed using electronic databases. In addition, nursing interventions, non-pharmacological treatments, and self-management programs relevant to patient health and nursing care were analyzed.
To further refine the program, focus group interviews were conducted with three patients who had been rehospitalized for pain management after discharge following lumbar spinal stenosis surgery. These interviews provided valuable insights into patients’ experiences and nursing needs, which were analyzed and incorporated into the program’s design. Additionally, a focus group interview was held with three nurses working in the spinal ward, including two orthopedic nurses with 6 and 7 years of experience, respectively, and one nurse manager with 11 years of experience, to explore needs related to postoperative care and practical considerations. The feedback from these nurses was also integrated into the program structure.
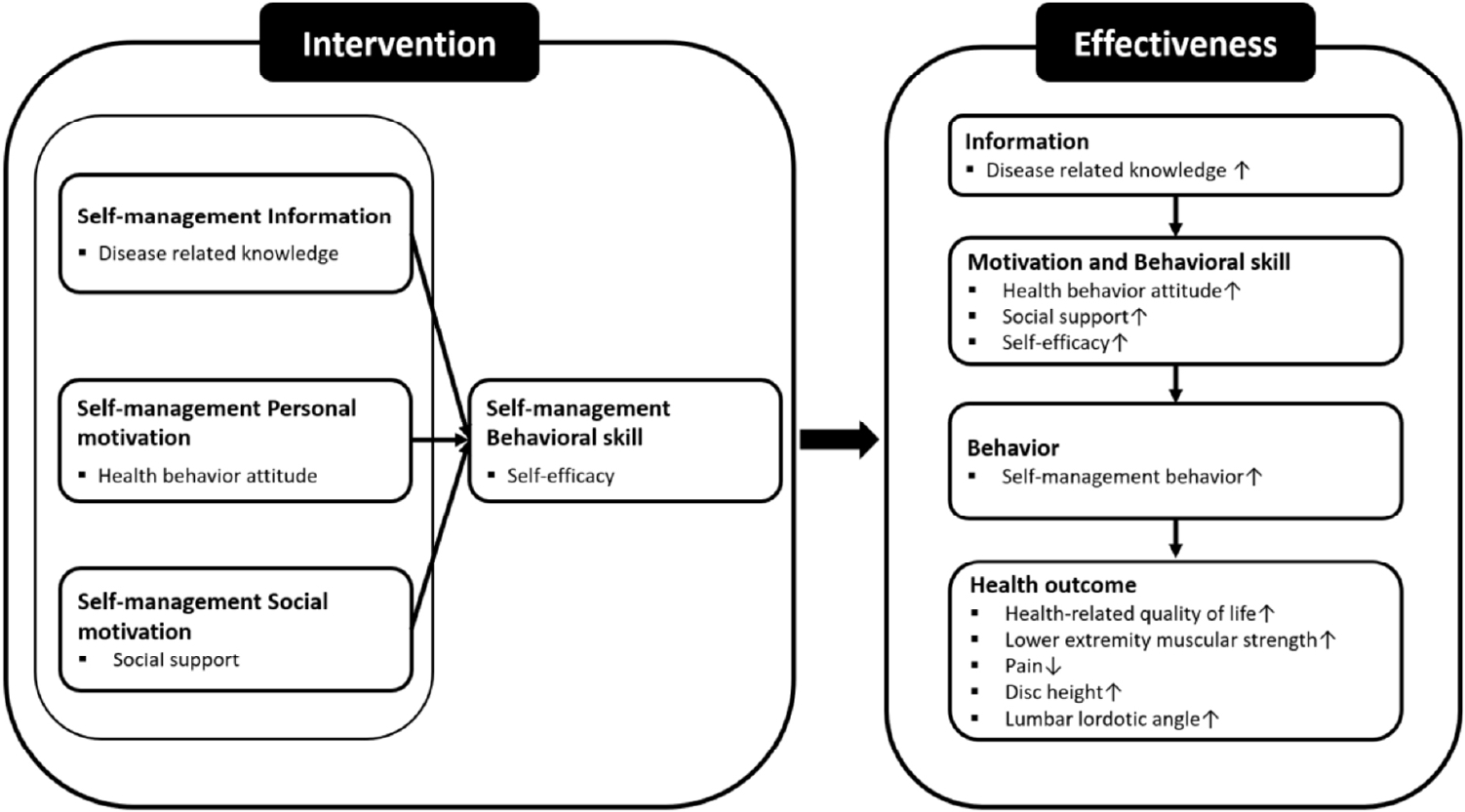
The conceptual framework for this study was based on the IMB model proposed by Fisher and Fisher [
10], which aims to facilitate changes in patients’ health behaviors by providing disease-related information, strengthening motivation, and enhancing behavioral skills to support long-term health maintenance (
Figure 1). Accordingly, the self-management program was structured to systematically deliver information, enhance motivation, and improve behavioral skills.
Specifically, a six-session program was conducted, spanning from the pre-hospitalization stage through post-discharge, integrating the IMB model into all aspects of self-management education. Program content included disease education, recovery exercises, guidance on correct posture, dietary management, medication management, and daily self-care.
The detailed structure of the self-management program is presented in
Table 1. Because the accessibility and quality of information can significantly influence health behavior [
22], visual aids such as images, illustrations, and videos were used to facilitate patient understanding. Expert opinions were incorporated to ensure the program’s sustainability, including the use of checklists and lumbar health journals that provided ongoing feedback. Additionally, educational booklet content was tailored to an estimated reading level equivalent to the 6th grade (approximately age 13 years), using simplified vocabulary, large fonts, and visual aids to ensure accessibility for older adults with varying literacy levels.
The self-management program was delivered as six individual 50-minute sessions over four weeks to patients undergoing lumbar spinal stenosis surgery. To assess effectiveness, post-intervention self-reported surveys, direct physical measurements, and medical record analyses were conducted. Throughout the six-session program, information provision, motivation enhancement, behavioral skill development, and facilitation of behavior change—rooted in the IMB model—were emphasized, covering disease education, recovery exercises, proper posture guidance, dietary management, medication management, and daily self-care practices.
The primary outcomes of the study included self-management information, motivation (both personal and social), behavioral skills, self-management behaviors, and HRQoL. The secondary outcomes were lower limb muscular strength, pain levels, intervertebral disc height, and lumbar lordosis angle.
The structure of the self-management program is detailed in
Table 1. As accessibility and quality of information influence health behavior [
22], visual learning tools such as illustrations, photographs, and videos were employed for patient education. Expert recommendations underscored the importance of patient-driven self-management to ensure ongoing engagement in self-care practices. To reinforce long-term adherence, checklists and lumbar health journals were provided to monitor and offer feedback. Furthermore, educational materials were adjusted for patients’ age-related needs, including larger font sizes and enhanced visual clarity.
This study was approved by the Institutional Review Board (IRB) of the Pukyong National University (No. 1041386-202207-HR-45-02). All measurement tools used were approved prior to the commencement of research.
To ensure ethical protection of participants, the purpose, methodology, and content of the study were fully explained prior to data collection. Participants were informed of their right to withdraw from the study at any time without penalty and were assured that their anonymity and confidentiality would be strictly maintained.
Given that study participants were inpatients and considered a vulnerable population, the self-management program was offered only to those who provided informed consent before hospitalization at the Spine Center outpatient clinic. The potential risks and benefits of participation were described in simple terms suited to each participant’s level of understanding. This explanation was provided before, during, and after the study to ensure full comprehension. Additionally, all participants were guaranteed that they would receive appropriate medical care and treatment regardless of their participation status. Those who completed the program received a small token of appreciation. Upon completion of the study, the control group was provided with educational booklets, access to the program, and a gift as an additional ethical consideration.
7. Data Analysis
Data were analyzed using the IBM SPSS version 23.0 (IBM Corp., Armonk, NY, USA). The reliability of the measurement tools was evaluated using Cronbach’s α and KR-20. Descriptive statistics, including frequency, percentage, mean, and standard deviation, were used to summarize participants’ general characteristics. Normality was assessed with the Shapiro–Wilk test.
Before the intervention, similarities between the experimental and control groups were analyzed using the independent t-test, the chi-square test, and the Fisher exact test. After the intervention, differences between the groups were assessed using the chi-square test, the independent t-test, and the Mann-Whitney U test. The significance level for evaluating the effectiveness of the IMB model–based self-management program for patients with lumbar spinal stenosis surgery was set at p<.05.
RESULTS
1. Homogeneity of General and Health Characteristics
A total of 58 participants were included in this study, with 30 in the experimental group and 28 in the control group. The mean age of participants was 66.79±7.21 years, with the experimental group averaging 67.60±6.76 years and the control group 65.93±7.69 years.
The experimental group comprised 11 men (36.7%) and 19 women (63.3%), while the control group included 11 men (39.3%) and 17 women (60.7%). Alcohol consumption was reported by eight participants (26.7%) in the experimental group and 12 participants (42.9%) in the control group. Furthermore, 26 participants (86.7%) in the experimental group and 22 participants (78.6%) in the control group reported maintaining a non-smoking status. Two or fewer comorbidities were present in 25 participants (83.3%) in the experimental group and 18 participants (64.3%) in the control group.
To assess the homogeneity of general characteristics, the chi-square test or Fisher exact test was performed. The results indicated that there were no statistically significant differences between the two groups in terms of age, gender, marital status, family cohabitation, religion, education level, employment status, income level, alcohol consumption, smoking status, or number of comorbidities.
Therefore, the experimental and control groups were considered homogeneous in terms of their general characteristics (
Table 2).
To assess homogeneity of the dependent variables at baseline, the t-test and Mann-Whitney U test were conducted for each outcome variable, including self-management information, personal and social motivation, behavioral skills, self-management behavior, HRQoL, lower limb strength, pain VAS scores (low back and leg), intervertebral disc height, and lumbar lordosis angle. The results showed no statistically significant differences between the experimental and control groups for any variable, confirming that the two groups were comparable prior to the intervention (
Table 3).
Following the intervention, the experimental group demonstrated statistically significant improvements compared to the control group in self-management information (
p<.001), personal and social motivation (
p=.002), behavioral skills (
p=.002), self-management behavior (
p=.003), and HRQoL (
p<.001). In addition, a significant increase in intervertebral disc height was observed (
p=.006). However, no statistically significant differences were found between the groups in lower limb strength, pain VAS scores, or lumbar lordosis angle, although both groups exhibited within-group improvements in these variables (
Table 4).
DISCUSSION
This study applied the IMB model proposed by Fisher and Fisher [
10] to develop and implement a six-session self-management program for patients undergoing lumbar spinal stenosis surgery. The results demonstrated that patients who participated in the program showed greater improvements in self-management information, motivation, behavioral skills, self-management behaviors, HRQoL, and intervertebral disc height than those who did not participate.
The findings showed a significant increase in self-management information scores in the experimental group after the intervention. This is consistent with studies by Kang and Kim [
23], who applied a knee osteoarthritis prevention program based on the IMB model, as well as Kim and Park [
24], who studied self-management programs for patients. Tsamlag et al. [
25] also identified improvement in information as a key factor for enhancing self-management behaviors in patients with osteoporosis. The increase in self-management information observed in this study is attributed to the use of easily understandable educational materials that incorporated images and illustrations explaining the definition, symptoms, and treatment process of lumbar spinal stenosis. Individualized education tailored to the participants’ cognitive levels, along with repeated sessions that combined theory, practice, and demonstration, contributed to reinforcing and correcting prior misconceptions. Given that most patients with lumbar spinal stenosis are older adults with long-standing habits and beliefs, the provision of accurate and accessible information is essential for promoting spinal health and sustaining disease-related knowledge.
This study also confirmed a significant effect of the program on self-management motivation, particularly personal motivation, measured through health beliefs and attitudes. In this study, personal motivation was assessed based on participants’ health beliefs and attitudes. The experimental group was encouraged to either write down or verbally express weekly self-management goals and actively work toward achieving them. This process of setting and accomplishing goals likely fostered a sense of achievement, which positively influenced participants’ health beliefs and attitudes after surgery. Additionally, the intervention was paced according to each patient’s readiness, and participants were guided to set realistic, personalized goals. These strategies contributed to enhancing motivation by promoting achievable progress tailored to each participant’s condition.
Self-management behavioral skills (self-efficacy) in the experimental group also increased significantly after the intervention. This result is consistent with findings by Jeong and Lee [
13], who focused on lumbar discectomy patients; Robinson [
26], who studied patients with hepatitis C; and Ameri et al. [
27], who examined patients with human immunodeficiency virus/acquired immune deficiency syndrome. The structured self-management program played a crucial role in enhancing self-efficacy by providing hands-on practice and continuous feedback, enabling patients to perform appropriate exercises. Kim and Hyun [
28] similarly reported that regular exercise enhances quality of life and psychological health, supporting the results of this study.
A significant increase in self-management behaviors was also observed in the experimental group after the intervention. These findings are in line with previous studies, including Jeong and Lee [
13], Kim and Park [
24], Ameri et al. [
27], and Wu et al. [
11]. The IMB model–based self-management program in this study effectively promoted positive changes in spinal health behaviors by providing self-management information, motivation, and self-efficacy improvement. These findings support the theoretical framework of the IMB model [
10], which posits that health behavior change and maintenance are facilitated when individuals acquire sufficient knowledge, motivation, and behavioral skills.
Lower limb strength, assessed using the STS5 test, did not show a statistically significant change after the intervention. Although the STS5 time in the experimental group decreased, the difference was not sufficient to support the hypothesis. This finding contrasts with previous studies that reported improvements in STS5 performance following resistance exercise programs for orthopedic patients [
29,
30], but aligns with research involving older surgical patients who received minimal physical intervention [
31,
32]. Additional evidence suggests that strength training enhances balance and helps prevent pain in older adults [
33]. The absence of a statistically significant improvement in this study may be related to age-related declines in muscle strength among patients with degenerative conditions such as lumbar spinal stenosis, which can lead to impaired balance and delayed sit-to-stand performance. These results underscore the need for ongoing physical activity and self-management to maintain functional mobility and prevent further deterioration.
Although VAS pain scores in the experimental group improved after the intervention, the difference did not reach statistical significance. Previous studies have reported reductions in low back pain through structured exercise programs for spinal surgery patients; however, this study did not include such targeted physical therapy components. Moreover, patients with lumbar spinal stenosis often expect complete relief from pain following surgery, yet persistent postoperative pain is common. This ongoing discomfort may influence patients’ subjective perceptions of pain and negatively affect their quality of life. These factors may have contributed to the lack of statistically significant findings related to pain in this study.
A statistically significant improvement in HRQoL was observed in the experimental group. This result is consistent with those of Kim and Kim [
12] and Kim et al. [
34], supporting the IMB model’s effectiveness in predicting behavioral changes related to disease prevention and improvements in HRQoL. In this study, sustained individualized education provided accurate disease information and goal-setting strategies, enabling participants to actively engage in self-care behaviors. However, as HRQoL is influenced by multiple factors, further interventions that enhance information, motivation, and behavioral skills should be explored [
6].
This study also found a statistically significant increase in intervertebral disc height in the experimental group. This result is consistent with the findings of Cho et al. [
5], who examined patients undergoing posterior lumbar interbody fusion surgery and found that disc height was maintained or increased postoperatively. Similarly, the study by Kim et al. [
35] demonstrated changes in disc height among patients with degenerative spinal diseases, further supporting the results of this study. While improvements in disc-related outcomes were observed, the effects on functional and symptomatic indicators were less clear. Although the experimental group showed improvements in lower limb strength and pain scores, these changes did not reach statistical significance. This may be due to the lack of intensive physical interventions, such as repeated resistance training or lumbar strengthening exercises using assistive devices, which have shown effectiveness in previous studies involving older adults in Korea. Additionally, the lack of prior studies on self-management programs specifically designed for patients after lumbar spinal stenosis surgery limits direct comparisons.
The IMB model–based self-management program developed in this study has several distinct features. It was designed to address the increasing number of older adults with lumbar spinal stenosis and to facilitate behavioral changes and long-term self-management. The program emphasized postoperative self-management and provided individualized education to enhance learning.
Unlike general self-management programs that primarily aim to promote overall health, this program systematically guided behavioral changes through the IMB model by combining disease-related information, counseling, and repeated interventions. The effectiveness of the program was objectively verified by evaluating not only self-management adherence but also objective physiological indicators, such as lower limb strength, intervertebral disc height, and lumbar lordosis angle.
This study had several limitations. First, it utilized a convenience sample of patients admitted to the orthopedic ward of a general hospital in Busan, which limits the generalizability of the findings. Second, some participants were hospitalized in the ward where the researcher was employed, which may have introduced potential bias. However, participation decisions were made prior to hospitalization, and the self-management program commenced in the outpatient spinal center. Therefore, it was not possible to predict which participants would later be admitted to the researcher’s ward. To minimize the risk of perceived coercion, informed consent was obtained, ensuring voluntary participation. Third, the intervention period was relatively short, restricting the ability to assess the long-term effects of the self-management program. Fourth, the study sample included only patients who had undergone surgery for lumbar spinal stenosis, thereby limiting the applicability of the findings to non-surgical populations. Fifth, no statistically significant improvements were observed in physiological indicators such as lower limb strength and functional movement. This may be attributed to age-related physical limitations and the absence of structured physical training within the intervention.
Future research should assess the long-term effects of self-management behaviors and consider developing similar interventions for non-surgical patients with lumbar spinal stenosis. As decreased muscle strength in older adults may pose a potential risk, further studies are also needed to examine the effectiveness of self-management programs in improving lower limb strength and functional mobility.
CONCLUSION
This study implemented a six-session self-management program based on the IMB model for patients undergoing lumbar spinal stenosis surgery and confirmed its effectiveness. The program significantly improved self-management information, motivation, behavioral skills, self-management behaviors, HRQoL, and intervertebral disc height in the experimental group.
Following the program, participants demonstrated behavioral changes such as posture correction, brace management, regular exercise, and lifestyle modifications. Furthermore, repeated education and demonstrations played a key role in enhancing learning outcomes and patient satisfaction.
The IMB model-based self-management program developed in this study could serve as an effective nursing intervention to improve the HRQoL of patients undergoing lumbar spinal stenosis surgery by integrating information, motivation, and behavioral skill strategies to promote sustainable self-management behaviors.
-
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
-
AUTHORSHIP
Study conception and/or design acquisition - GYC and MKS; analysis and interpretation of the data - MKS; interpretation of the data - MKS; drafting or critical revision of the manuscript for important intellectual content - GYC and MKS.
-
FUNDING
None.
-
ACKNOWLEDGEMENT
This article is a revision of the Mi Kyung Seo’s doctoral dissertation from Pukyong National University.
-
DATA AVAILABILITY STATEMENT
The data can be obtained from the corresponding authors.
Figure 1.Conceptual framework for this study.
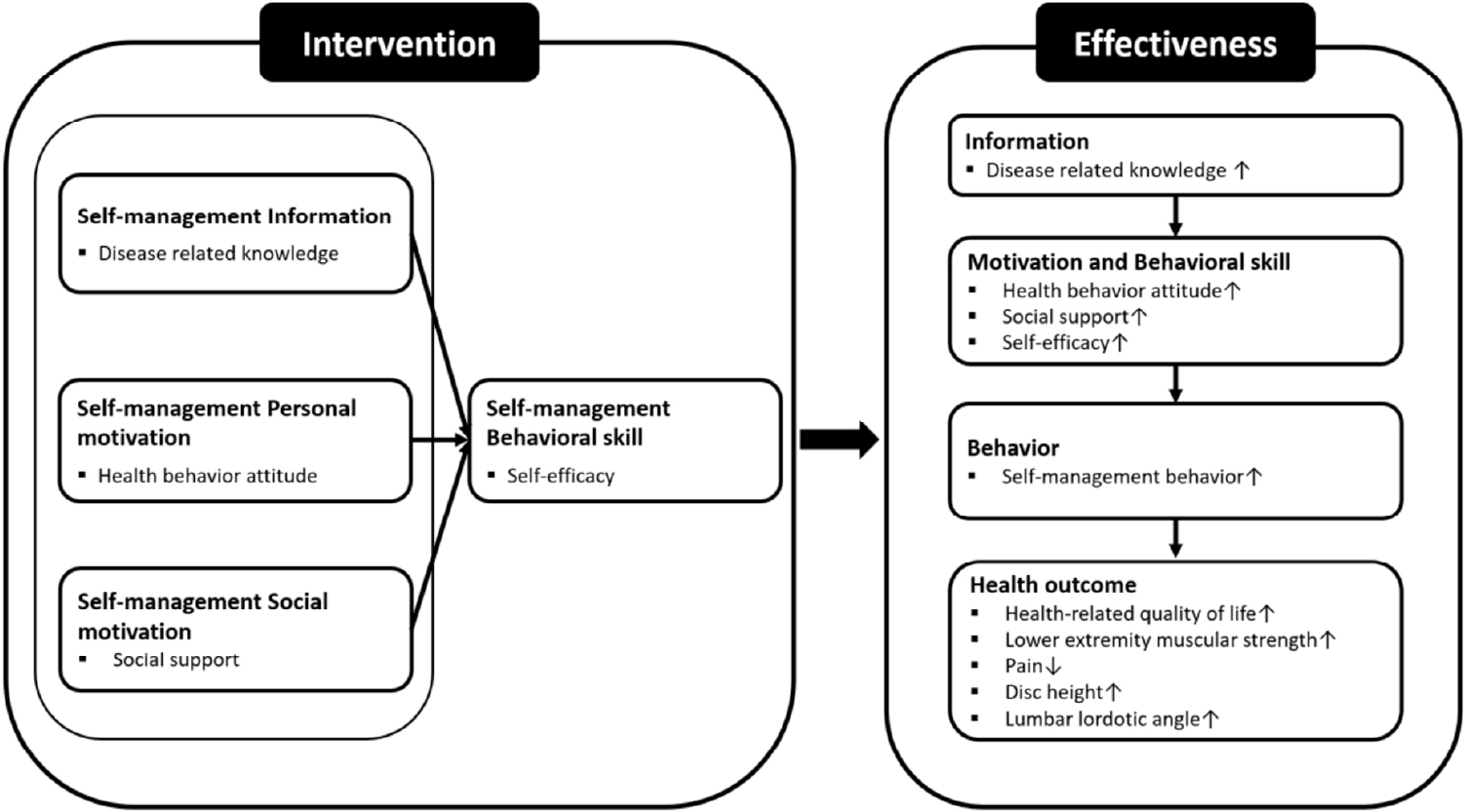
Table 1.Self-Management Program for Patients Undergoing Lumbar Spinal Stenosis Surgery Based on the IMB Model
|
Session |
Contents |
|
Strategies |
Time (min) |
|
Information |
Motivation |
|
Behavioral skills |
|
Disease-related knowledge |
Personal |
Social |
Self-efficacy |
|
1 |
Lumbar spinal stenosis |
Goal setting |
Provide a video of encouraging lumbar spinal stenosis surgery patients |
Goal achievement check |
Face-to-face† (meeting individually) (1:1) |
50 |
|
2 |
Preoperative self-management |
Self-management checklist for lumbar spinal stenosis surgery check |
Share experiences of lumbar spinal stenosis surgery patients |
Practice of program check |
Counseling†
|
50 |
|
3 |
Postoperative self-management |
|
Q&A |
Provide feedback |
Practices†
|
50 |
|
4 |
Ambulation and exercise |
|
Help with problem-solving methods |
True/false quiz |
Multimedia |
50 |
|
5 |
Re-education on self-management for lumbar spinal stenosis |
|
|
|
Self-management booklet |
50 |
|
6 |
Self-management education for hospital discharge |
|
|
|
|
50 |
Table 2.Homogeneity of the Participants’ General and Health Characteristics (N=58)
|
Characteristics |
Categories |
Exp. (n=30) |
Con. (n=28) |
χ2 or Z |
p
|
|
n (%) or M±SD |
|
Age (year)†
|
50–59 |
3 (10.0) |
5 (17.9) |
0.80 |
.769 |
|
60–69 |
16 (53.3) |
14 (50.0) |
|
≥70 |
11 (36.7) |
9 (32.1) |
|
67.60±6.76 |
65.93±7.69 |
|
Sex |
Male |
11 (36.7) |
11 (39.3) |
0.04 |
.837 |
|
Female |
19 (63.3) |
17 (60.7) |
|
Marital status†
|
Married |
26 (86.7) |
26 (92.9) |
0.60 |
.671 |
|
Single |
4 (13.3) |
2 (7.1) |
|
Living with†
|
Spouse |
5 (16.7) |
12 (42.9) |
5.99 |
.116 |
|
Family |
17 (56.7) |
9 (32.1) |
|
Child |
4 (13.3) |
5 (17.9) |
|
Alone |
4 (13.3) |
2 (7.1) |
|
Religion |
Yes |
20 (66.7) |
16 (57.1) |
0.56 |
.455 |
|
No |
10 (33.3) |
12 (42.9) |
|
Education |
≤Middle school |
19 (63.4) |
14 (50.0) |
1.06 |
.306 |
|
≥High school diploma |
11 (36.6) |
14 (50.0) |
|
Employed |
Yes |
12 (40.0) |
10 (35.7) |
0.11 |
.737 |
|
No |
18 (60.0) |
18 (64.3) |
|
Income (10,000 won/months) |
<200 |
20 (66.7) |
13 (46.4) |
2.42 |
.120 |
|
≥200 |
10 (33.3) |
15 (53.6) |
|
Alcohol |
Yes |
8 (26.7) |
12 (42.9) |
1.68 |
.195 |
|
No |
22 (73.3) |
16 (57.1) |
|
Smoking†
|
Yes |
4 (13.3) |
6 (21.4) |
0.67 |
.499 |
|
No |
26 (86.7) |
22 (78.6) |
|
No. of comorbidities‡
|
≤2 |
25 (83.3) |
18 (64.3) |
2.70 |
.098 |
|
≥3 |
5 (16.7) |
10 (35.7) |
Table 3.Homogeneity of Dependent Variables of Participants (N=58)
|
Variables |
Exp. (n=30) |
Con. (n=28) |
t or Z |
p
|
|
n (%) or M±SD |
|
Information†
|
9.00±1.55 |
9.07±2.43 |
–0.42 |
.678 |
|
Motivation |
|
|
|
|
|
Personal |
3.37±0.23 |
3.38±0.32 |
–0.17 |
.865 |
|
Social |
3.36±0.73 |
3.53±0.56 |
–0.98 |
.331 |
|
Behavioral skills |
3.03±0.76 |
2.85±0.78 |
0.91 |
.368 |
|
Behaviors†
|
3.41±0.62 |
3.26±0.48 |
–0.51 |
.612 |
|
HRQoL†
|
0.53±0.28 |
0.64±0.21 |
–1.09 |
.276 |
|
Lower extremity muscular strength |
41.98±11.41 |
41.02±9.42 |
0.35 |
.730 |
|
VAS score of LBP†
|
7.70±0.84 |
7.54±1.07 |
–0.20 |
.779 |
|
VAS score of leg pain†
|
5.17±1.26 |
5.79±1.55 |
–1.41 |
.147 |
|
Disc height†
|
0.56±0.11 |
0.51±0.13 |
–1.01 |
.315 |
|
Lumbar lordotic angle†
|
66.73±5.95 |
62.36±8.59 |
–1.87 |
.062 |
Table 4.Comparison of Dependent Variables between the Experimental and Control Groups (N=58)
|
Variables |
Categories |
Pretest |
Posttest |
Differences |
t or Z |
p
|
|
M±SD |
|
Information |
Exp. |
9.00±1.55 |
12.10±0.66 |
3.10±1.69 |
4.01 |
<.001 |
|
Con. |
9.07±2.43 |
9.68±1.39 |
0.61±2.60 |
|
Motivation |
Personal |
Exp. |
3.37±0.23 |
3.77±0.61 |
0.40±0.56 |
3.34 |
.002 |
|
Con. |
3.38±0.32 |
3.40±0.25 |
0.02±0.24 |
|
Social |
Exp. |
3.36±0.73 |
3.96±0.40 |
0.60±0.58 |
3.29 |
.002 |
|
Con. |
3.53±0.56 |
3.69±0.45 |
0.16±0.41 |
|
Behavior skills†
|
Exp. |
3.03±0.76 |
4.09±0.68 |
1.06±0.70 |
3.32 |
.002 |
|
Con. |
2.85±0.78 |
3.58±0.78 |
0.73±0.92 |
|
Behaviors |
Exp. |
3.41±0.62 |
4.17±0.39 |
0.76±0.55 |
2.94 |
.003 |
|
Con. |
3.26±0.48 |
3.75±0.57 |
0.49±0.69 |
|
HRQoL†
|
Exp. |
0.53±0.28 |
0.92±0.09 |
0.39±0.29 |
3.79 |
<.001 |
|
Con. |
0.64±0.21 |
0.78±0.11 |
0.14±0.22 |
|
Lower extremity muscular strength |
Exp. |
41.98±11.41 |
30.10±6.26 |
–11.89±9.83 |
–1.19 |
.239 |
|
Con. |
41.02±9.42 |
32.09±6.45 |
–8.93±9.03 |
|
VAS score of LBP†
|
Exp. |
7.70±0.84 |
2.33±0.76 |
-5.37±1.19 |
–1.55 |
.122 |
|
Con. |
7.54±1.07 |
2.82±1.06 |
–4.71±1.33 |
|
VAS score of leg pain†
|
Exp. |
5.17±1.26 |
2.47±0.78 |
–2.70±1.21 |
–1.96 |
.050 |
|
Con. |
5.79±1.55 |
2.32±0.91 |
–3.46±1.37 |
|
Disc height†
|
Exp. |
0.56±0.11 |
0.66±0.13 |
0.10±0.11 |
2.75 |
.006 |
|
Con. |
0.51±0.13 |
0.56±0.12 |
0.05±0.11 |
|
Lumbar lordotic angle†
|
Exp. |
66.73±5.95 |
67.51±7.13 |
0.59±6.35 |
–0.18 |
.858 |
|
Con. |
56.76±9.45 |
57.47±9.83 |
0.64±3.77 |
REFERENCES
- 1. National Health Insurance Service. Health checkup [Internet]. Wonju: National Health Insurance Service; 2021 [cited 2022 July 11]. Available from: http://www.nhis.or.kr
- 2. Kim SM, Lee SJ. The development and effect of a video education program on uncertainty and educational satisfaction among spinal surgery patients. J Muscle Joint Health. 2018;25(3):187-95. https://doi.org/10.5953/JMJH.2018.25.3.187
- 3. Seoul National University Hospital. 14% of patients with back spinal stenosis have to undergo reoperation within five years [Internet]. Seoul: Seoul National University Hospital; 2013 [cited 2022 August 11]. Available from: https://www.snuh.org/board/B015/view.do?bbs_no=4018&searchKey=&searchWord=&pageIndex=1
- 4. Jang YS, Jung SY. Factors related to quality of life of patients with failed back surgery syndrome. J Korean Acad Fundam Nurs. 2021;28(3):311-9. https://doi.org/10.7739/jkafn.2021.28.3.311
- 5. Cho KJ, Kim YT, Park SR, Hong SH. Restoration of lumbar lordosis after posterior lumbar interbody fusion with 4 degree cage in degenerative spinal disease. J Korean Soc Spine Surg. 2013;20(2):51-7. https://doi.org/10.4184/jkss.2013.20.2.51
- 6. Bae CW, Lee JB. Effect of functional adjustment procedure on pain, dysfunction and, health-related quality of life in patients with chronic low back pain. J Korean Soc Phys Med. 2020;15(2):109-20. https://doi.org/10.13066/kspm.2020.15.2.109
- 7. Song MY, Jo HG, Sul JU, Leem J. Proposal of east-west integrative medicine manual for rehabilitation after shoulder surgery. J Korean Med Rehabi. 2018;28(1):109-20. https://doi.org/10.18325/jkmr.2018.28.1.109
- 8. Kim HJ, Lee HM, Kim HS, Moon ES, Park JO, Lee KJ, et al. Life expectancy after lumbar spine surgery: one- to eleven-year follow-up of 1015 patients. Spine (Phila Pa 1976). 2008;33(19):2116-21. https://doi.org/10.1097/BRS.0b013e31817e1022
- 9. Shin IH, Cho KS. Effects of the back pain management program on patients with chronic low back pain. J Muscle Joint Health. 2014;21(2):114-24. https://doi.org/10.5953/JMJH.2014.21.2.114
- 10. Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455-74. https://doi.org/10.1037/0033-2909.111.3.455
- 11. Wu Q, Jiang Z, Su T, Dai Y, Huang D, Lai R, et al. The Design of elderly fracture rehabilitation software based on "Information-Motivation-Behavioral Skills Model". Stud Health Technol Inform. 2018;250:234. https://doi.org/10.3233/978-1-61499-872-3-234
- 12. Kim JS, Kim CJ. Effect of a physical activity promoting program based on the IMB model on obese-metabolic health outcomes among obese older adults with knee osteoarthritis. J Korean Acad Nurs. 2020;50(2):271-85. https://doi.org/10.4040/jkan.2020.50.2.271
- 13. Jeong JH, Lee HK. Effects of self-care program on exercise performance self-efficay, self-care knowledge, self-care performance in patients with lumbar discectomy. J Korean Appl Sci Technol. 2021;38(3):891-902. https://doi.org/10.12925/jkocs.2021.38.3.891
- 14. Torabi MR, Seo DC, Jeng I. Alternate forms of health attitude scale. Am J Health Behav. 2004;28(2):166-72. https://doi.org/10.5993/ajhb.28.2.7
- 15. Kim HR. The effects of the factors influencing the physical health behaviors on people with mental illness based on the theory of triadic influence [dissertation]. Seoul: Ewha Womans University; 2006.
- 16. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30-41. https://doi.org/10.1207/s15327752jpa5201_2
- 17. Shin JS, Lee YB. The effects of social supports on psychosocial well-being of the unemployed. Korean J Soc Welf. 1999;37:241-69.
- 18. Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60-6. https://doi.org/10.1080/02701367.1992.10607557
- 19. Lee PS, Chang SO. The study on the effect of stage based exercise motivational intervention program for the elderly. J Korean Acad Nurs. 2017;31(5):818-34. https://doi.org/10.4040/jkan.2001.31.5.818
- 20. Nam HS, Kim KY, Kwon SS, Koh KW, Poul K. EQ-5D Korean valuation study using time trade off method. Seoul: Korea Centers for Disease Control and Prevention; 2007.
- 21. Farfan HF. Mechanical disorders of the low back. Philadelphia: Lea & Febiger; 1973.
- 22. Williams SL, DiMatteo MR, Haskard KB. Psychosocial barriers to adherence and lifestyle change. In: Shumaker SA, Ockene JK, Riekert KA, editors. The handbook of health behavior change. 3rd ed. New York: Springer Publishing Company; 2009. p. 445-61.
- 23. Kang GS, Kim JS. Development and effects of mobile app-based prevention program of knee osteoarthritis for obese middle-aged women based on IMB model. J Korean Gerontol Soc. 2023;43(1):109-28. https://doi.org/10.31888/JKGS.2023.43.1.109
- 24. Kim YI, Park JS. Development and effects of mobile app-based prevention program of knee osteoarthritis for obese middle-aged women based on IMB model. J Korean Acad Community Health Nurs. 2017;28(1):55-68. https://doi.org/10.12799/jkachn.2017.28.1.55
- 25. Tsamlag L, Wang H, Shen Q, Shi Y, Zhang S, Chang R, et al. Applying the information-motivation-behavioral model to explore the influencing factors of self-management behavior among osteoporosis patients. BMC Public Health. 2020;20(1):198. https://doi.org/10.1186/s12889-020-8292-x
- 26. Robinson WT. Adaptation of the information-motivation-behavioral skills model to needle sharing behaviors and hepatitis C risk: a structural equation model. SAGE Open. 2017;7(1):2158244016666126. https://doi.org/10.1177/2158244016666126
- 27. Ameri M, Movahed E, Farokhzadian J. Effect of information, motivation, and behavioral skills model on adherence to medication, diet, and physical activity in HIV/ADIS patients: a health promotion strategy. J Educ Health Promot. 2020;9:317. https://doi.org/10.4103/jehp.jehp_188_20
- 28. Kim JS, Hyun HJ. Effect of program promoting intention to exercise performance based theory of planned behavior in the elderly. J Korean Biol Nurs Sci. 2015;17(1):1-10. https://doi.org/10.7586/jkbns.2015.17.1.1
- 29. Kulig K, Beneck GJ, Selkowitz DM, Popovich JM Jr, Ge TT, Flanagan SP, et al. An intensive, progressive exercise program reduces disability and improves functional performance in patients after single-level lumbar microdiskectomy. Phys Ther. 2009;89(11):1145-57. https://doi.org/10.2522/ptj.20080052
- 30. Selkowitz DM, Kulig K, Poppert EM, Flanagan SP, Matthews ND, Beneck GJ, et al. The immediate and long-term effects of exercise and patient education on physical, functional, and quality-of-life outcome measures after single-level lumbar microdiscectomy: a randomized controlled trial protocol. BMC Musculoskelet Disord. 2006;7:70. https://doi.org/10.1186/1471-2474-7-70
- 31. Yu S, Lee S, Kim M, Park DS. The feasibility study of sit-to-stand and stand-to-sit assistive chair for elderly. Phys Ther Rehabil Sci. 2022;11:591-7. https://doi.org/10.14474/ptrs.2022.11.4.591
- 32. An JH. The effects of lumbar extension strength and lumbar pain reduction after lumbar muscle strength exercise for 8 weeks in lumbar disease patients. J Korean Soc Wellness. 2011;6(2):275-84.
- 33. Cho HM. Systematic review of fall prediction of the elderly using sit-to-stand-five-times test [master’s thesis]. Seoul: Konkuk University; 2019.
- 34. Kim CJ, Kang HS, Kim JS, Won YY, Schlenk EA. Predicting physical activity and cardiovascular risk and quality of life in adults with osteoarthritis at risk for metabolic syndrome: a test of the information-motivation-behavioral skills model. Nurs Open. 2020;7(4):1239-48. https://doi.org/10.1002/nop2.500
- 35. Kim WJ, Kang JW, Park JG, Park KY, Sung HI, Choy WS. Radiological and clinical analysis of degenerative lumbar retrolisthesis-comparative study of degenerative spondylolisthesis. J Korean Soc Spine Surg. 2005;12(4):338-43. https://doi.org/10.4184/jkss.2005.12.4.338