1Department of Nursing, Inha University, Inha University Hospital, Incheon
2Inha University Hospital, Incheon
3Department of Nursing, Inha University, Incheon, Korea
© 2012 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Extrinsic | Intrinsic factors | Coefficient estimates | SMC | ||
|---|---|---|---|---|---|
| Direct (T-value) | Indirect (T-value)† | Total (T-value) | |||
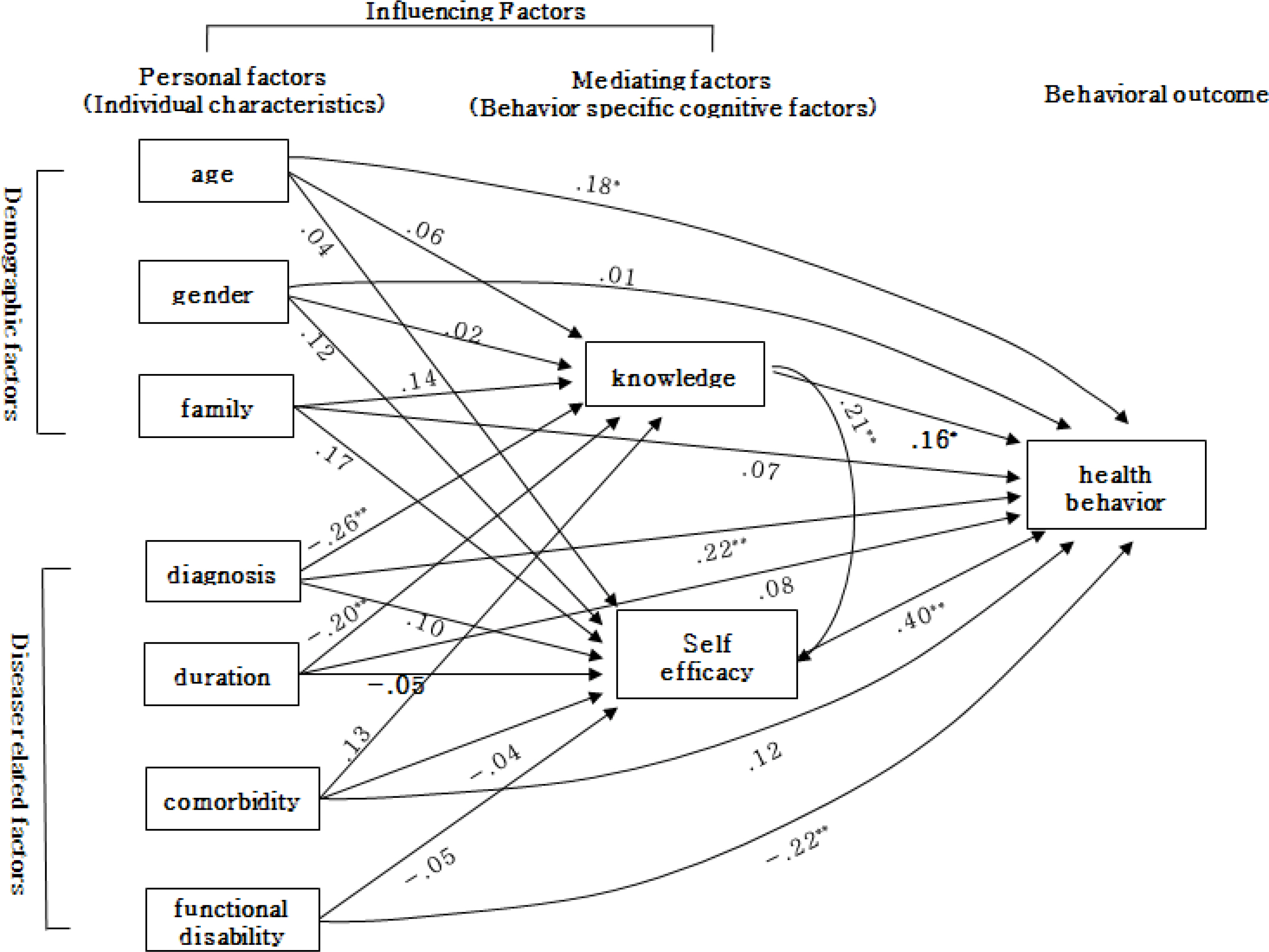
| Knowledge related to health | Age | .06 (0.50) | - | .06 (0.50) | .11 |
| Gender‡ | .02 (0.24) | - | .02 (0.24) | ||
| Living together with family§ | .14 (1.34) | - | .14 (1.34) | ||
| Diagnosis|| | -.26 (-2.59)∗∗ | - | -.26 (-2.59)∗∗ | ||
| Duration of illness | -.20 (-1.98)∗∗ | - | -.20 (-1.98)∗∗ | ||
| Comorbidity¶ | .13 (1.21) | - | .13 (1.21) | ||
| Self-efficacy | Age | .04 (0.36) | .01 (0.49) | .05 (0.46) | .10 |
| Gender | .12 (1.19) | .01 (0.24) | .13 (1.21) | ||
| Living together with family | .17 (1.55) | .03 (1.14) | .20 (1.81)∗ | ||
| Diagnosis | .10 (0.98) | -.05 (-1.61) | .05 (0.46) | ||
| Duration of diagnosis | -.05 (-0.51) | -.04 (-1.45) | -.09 (-0.91) | ||
| Comorbidity | -.04 (-0.39) | .03 (1.05) | -.01 (-0.14) | ||
| Functional disability | -.05 (-0.52) | - | -.05 (-0.52) | ||
| Knowledge related to health | .21 (2.13)∗∗ | - | .21 (2.13)∗∗ | ||
| Health behavior | Age | .18 (1.89)∗ | .03 (0.56) | .21 (1.93)∗ | .36 |
| Gender | .01 (0.03) | .05 (1.11) | .06 (0.57) | ||
| Living together with family | .07 (0.71) | .10 (1.90)∗ | .17 (1.61) | ||
| Diagnosis | -.22 (-2.46)∗∗ | .02 (0.42) | .20 (2.02)∗∗ | ||
| Duration of illness | .08 (0.87) | -.07 (-1.37) | .01 (0.08) | ||
| Comorbidity | .12 (1.30) | .01 (0.28) | .13 (1.29) | ||
| Functional disability | -.22 (-2.58)∗∗ | -.02 (-0.52) | -.24 (-2.56)∗∗ | ||
| Knowledge related to health | .16 (1.84)∗ | .08 (1.95)∗ | .24 (2.61)∗∗ | ||
| Self-efficacy | .40 (4.79)∗∗ | - | .40 (4.79)∗∗ | ||
∗T≥1.64, p≤.05; ∗∗T≥1.96, p≤.01).
†Mediating effect SMC=squared multiple correlation;
‡1) male, 2) female;
§1) no (living alone), 2) yes (living together with family);
||1) cerebral infarction, 2) cerebral hemorrhage;
¶1) no (without history of hypertension or diabetes mellitus), 2) yes (with history of hypertension or diabetes mellitus).

Descriptive Statistics of Subjects' Characteristics (N=105)
| Characteristics | Categories | n (%) or M±SD |
|---|---|---|
| Age (year) | 60.9±13.85 | |
| Age group (year) | >50 | 17 (16.2) |
| 50~59 | 30 (28.6) | |
| ≤60 | 58 (55.2) | |
| Gender | Male | 58 (55.2) |
| Female | 47 (54.8) | |
| Living together with family | Yes | 91 (86.7) |
| No | 14 (13.3) | |
| Diagnosis | CI | 72 (68.6) |
| CH | 33 (31.4) | |
| Duration of stroke (year) | 1.45±1.55 | |
| Comorbidity (diabetes or hypertension) | Yes | 68 (64.8) |
| No | 37 (35.2) | |
| Functional disability | 3.01±1.09 |
CI=cerebral infarction; CH=cerebral hemorrhage.
Parameters Estimates of the Hypothetical Model of Influencing and Mediating Factors of Health Behavior for Stroke Patients
| Extrinsic | Intrinsic factors | Coefficient estimates | SMC | ||
|---|---|---|---|---|---|
| Direct (T-value) | Indirect (T-value) |
Total (T-value) | |||
| Knowledge related to health | Age | .06 (0.50) | - | .06 (0.50) | .11 |
| Gender |
.02 (0.24) | - | .02 (0.24) | ||
| Living together with family |
.14 (1.34) | - | .14 (1.34) | ||
| Diagnosis |
-.26 (-2.59)∗∗ | - | -.26 (-2.59)∗∗ | ||
| Duration of illness | -.20 (-1.98)∗∗ | - | -.20 (-1.98)∗∗ | ||
| Comorbidity |
.13 (1.21) | - | .13 (1.21) | ||
| Self-efficacy | Age | .04 (0.36) | .01 (0.49) | .05 (0.46) | .10 |
| Gender | .12 (1.19) | .01 (0.24) | .13 (1.21) | ||
| Living together with family | .17 (1.55) | .03 (1.14) | .20 (1.81)∗ | ||
| Diagnosis | .10 (0.98) | -.05 (-1.61) | .05 (0.46) | ||
| Duration of diagnosis | -.05 (-0.51) | -.04 (-1.45) | -.09 (-0.91) | ||
| Comorbidity | -.04 (-0.39) | .03 (1.05) | -.01 (-0.14) | ||
| Functional disability | -.05 (-0.52) | - | -.05 (-0.52) | ||
| Knowledge related to health | .21 (2.13)∗∗ | - | .21 (2.13)∗∗ | ||
| Health behavior | Age | .18 (1.89)∗ | .03 (0.56) | .21 (1.93)∗ | .36 |
| Gender | .01 (0.03) | .05 (1.11) | .06 (0.57) | ||
| Living together with family | .07 (0.71) | .10 (1.90)∗ | .17 (1.61) | ||
| Diagnosis | -.22 (-2.46)∗∗ | .02 (0.42) | .20 (2.02)∗∗ | ||
| Duration of illness | .08 (0.87) | -.07 (-1.37) | .01 (0.08) | ||
| Comorbidity | .12 (1.30) | .01 (0.28) | .13 (1.29) | ||
| Functional disability | -.22 (-2.58)∗∗ | -.02 (-0.52) | -.24 (-2.56)∗∗ | ||
| Knowledge related to health | .16 (1.84)∗ | .08 (1.95)∗ | .24 (2.61)∗∗ | ||
| Self-efficacy | .40 (4.79)∗∗ | - | .40 (4.79)∗∗ | ||
∗T≥1.64, p≤.05; ∗∗T≥1.96, p≤.01).
†Mediating effect SMC=squared multiple correlation;
‡1) male, 2) female;
§1) no (living alone), 2) yes (living together with family);
||1) cerebral infarction, 2) cerebral hemorrhage;
¶1) no (without history of hypertension or diabetes mellitus), 2) yes (with history of hypertension or diabetes mellitus).
CI=cerebral infarction; CH=cerebral hemorrhage.
∗T≥1.64, Mediating effect SMC=squared multiple correlation; 1) male, 2) female; 1) no (living alone), 2) yes (living together with family); 1) cerebral infarction, 2) cerebral hemorrhage; 1) no (without history of hypertension or diabetes mellitus), 2) yes (with history of hypertension or diabetes mellitus).