1Doctoral Student, College of Nursing, Seoul National University, Seoul
2Assistant Professor, College of Nursing, Seoul National University, Seoul, Korea
Copyright © 2017 Korean Society of Adult Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
| Variables | PSQI | FSS | BDI | S-STAI | T-STAI |
|---|---|---|---|---|---|
| PSQI | 1 | ||||
| FSS | .39 (<.001) | 1 | |||
| BDI | .44 (<.001) | .37 (<.001) | 1 | ||
| S-STAI | .23 (.001) | .28 (<.001) | .59 (<.001) | 1 | |
| T-STAI | .34 (<.001) | .41 (<.001) | .69 (<.001) | .72 (<.001) | 1 |

Comparisons of General Characteristics by Sleep Quality (N=208)
| Variables | Categories | Total (N=208) | Good sleepers (n=115) | Bad sleepers (n=93) | x2 or t | p |
|---|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | ||||
| Gender | Male | 63 (30.3) | 38 (33.0) | 25 (26.9) | 0.93 | .336 |
| Female | 145 (69.7) | 77 (67.0) | 68 (73.1) | |||
| Age (year) | 20~29 | 51 (24.5) | 30 (26.1) | 10 (10.8) | 0.38 | .998 |
| 30~39 | 52 (25.0) | 26 (22.6) | 23 (24.7) | |||
| 40~49 | 52 (25.0) | 30 (26.1) | 34 (36.6) | |||
| 50~60 | 53 (25.5) | 29 (25.2) | 26 (28.0) | |||
| 40.56±11.72 | 40.52±11.60 | 40.61±11.94 | -0.05 | .959 | ||
| Education level completed | ≥High school | 192 (92.3) | 105 (91.3) | 87 (93.5) | 0.30 | .582 |
| <High school | 16 (7.7) | 10 (8.7) | 6 (6.5) | |||
| Job | Employed | 144 (69.2) | 80 (69.6) | 64 (68.8) | 0.10 | .761 |
| Unemployed | 64 (30.8) | 35 (30.4) | 29 (31.2) | |||
| Living status | Live alone | 51 (24.5) | 27 (23.5) | 24 (25.8) | 0.50 | .823 |
| Live with family | 157 (75.5) | 88 (76.5) | 69 (74.2) | |||
| Economic status | High | 6 (2.9) | 2 (1.7) | 4 (4.3) | 0.73 | .833 |
| Middle | 190 (91.3) | 106 (92.2) | 84 (90.3) | |||
| Low | 12 (5.8) | 7 (6.1) | 5 (5.4) | |||
| Presence of chronic disease | Yes | 57 (27.4) | 27 (23.5) | 30 (32.3) | 2.14 | .144 |
| No | 151 (72.6) | 88 (76.5) | 63 (67.7) | |||
| BMI (kg/m2) | 23.39±3.33 | 23.54±3.69 | 23.22±2.83 | 0.71 | .476 | |
| Body fat mass (%) | 27.33±7.09 | 27.53±7.54 | 27.07±6.52 | 0.47 | .643 |
Good sleepers=Pittsburgh sleep quality index score ≤5; Bad sleeper=Pittsburgh sleep quality index score>5; BMI=body mass index.
Comparisons of Sleep Quality (N=208)
| PSQI Subcategories | Range | Total (N=208) | Good sleepers (n=115) | Bad sleepers (n=93) | x2 or t | p |
|---|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | ||||
| Total PSQI score | 0~21 | 5.65±3.15 | 3.46±1.32 | 8.35±2.60 | -16.50 | <.001 |
| Subjective sleep quality | 0~3 | 1.20±0.74 | 0.83±0.53 | 1.65±0.72 | -9.09 | <.001 |
| Sleep latency (minute) | 0 (≤15) | 120 (57.7) | 85 (73.9) | 35 (37.6) | 52.58 | <.001 |
| 1 (16~30) | 60 (28.8) | 29 (25.2) | 31 (33.3) | |||
| 2 (31~59) | 20 (9.6) | 1 (0.9) | 19 (20.4) | |||
| 3 (≥60) | 8 (3.8) | ․ | 8 (8.6) | |||
| 0~3 | 1.03±0.95 | 0.54±0.61 | 1.65±0.93 | -9.99 | <.001 | |
| Sleep duration (hour) | 0 (≥7) | 64 (30.8) | 54 (47.0) | 10 (10.8) | 21.12 | <.001 |
| 1 (6~7) | 71 (34.1) | 48 (41.7) | 23 (24.7) | |||
| 2 (5~6) | 44 (21.2) | 10 (8.7) | 34 (36.6) | |||
| 3 (<5) | 29 (13.9) | 3 (2.6) | 26 (28.0) | |||
| 0~3 | 1.18±1.02 | 0.67±0.75 | 1.82±0.97 | -9.40 | <.001 | |
| Habitual sleep efficiency | 0~3 | 0.46±0.85 | 0.06±0.24 | 0.95±1.06 | -7.92 | <.001 |
| Sleep disturbance | 0~3 | 1.11±1.08 | 0.73±0.85 | 1.58±1.16 | -5.92 | <.001 |
| Frequency of taking sleeping pill | 0 (0) | 203 (97.6) | 115 (100.0) | 88 (94.6) | 584.65 | <.001 |
| 1 (≤1/week) | 1 (0.5) | ․ | 1 (1.1) | |||
| 2 (1~2/week) | 2 (1.0) | ․ | 2 (2.2) | |||
| 3 (≥3/week) | 2 (1.0) | ․ | 2 (2.2) | |||
| 0~3 | 0.05±0.36 | 0.00±0.00 | 0.12±0.53 | -2.16 | .034 | |
| Daytime dysfunction | 0~3 | 0.52±0.80 | 0.30±0.58 | 0.81±0.95 | -4.56 | <.001 |
PSQI=PittsburGh Sleep Quality Index.
Heart Rate Variability, Fatigue, Depression, and State Trait Anxiety by Sleep Quality (N=208)
| Variables | Total (N=208) | Good sleepers (n=115) | Bad sleepers (n=93) | t | p |
|---|---|---|---|---|---|
| M±SD | M±SD | M±SD | |||
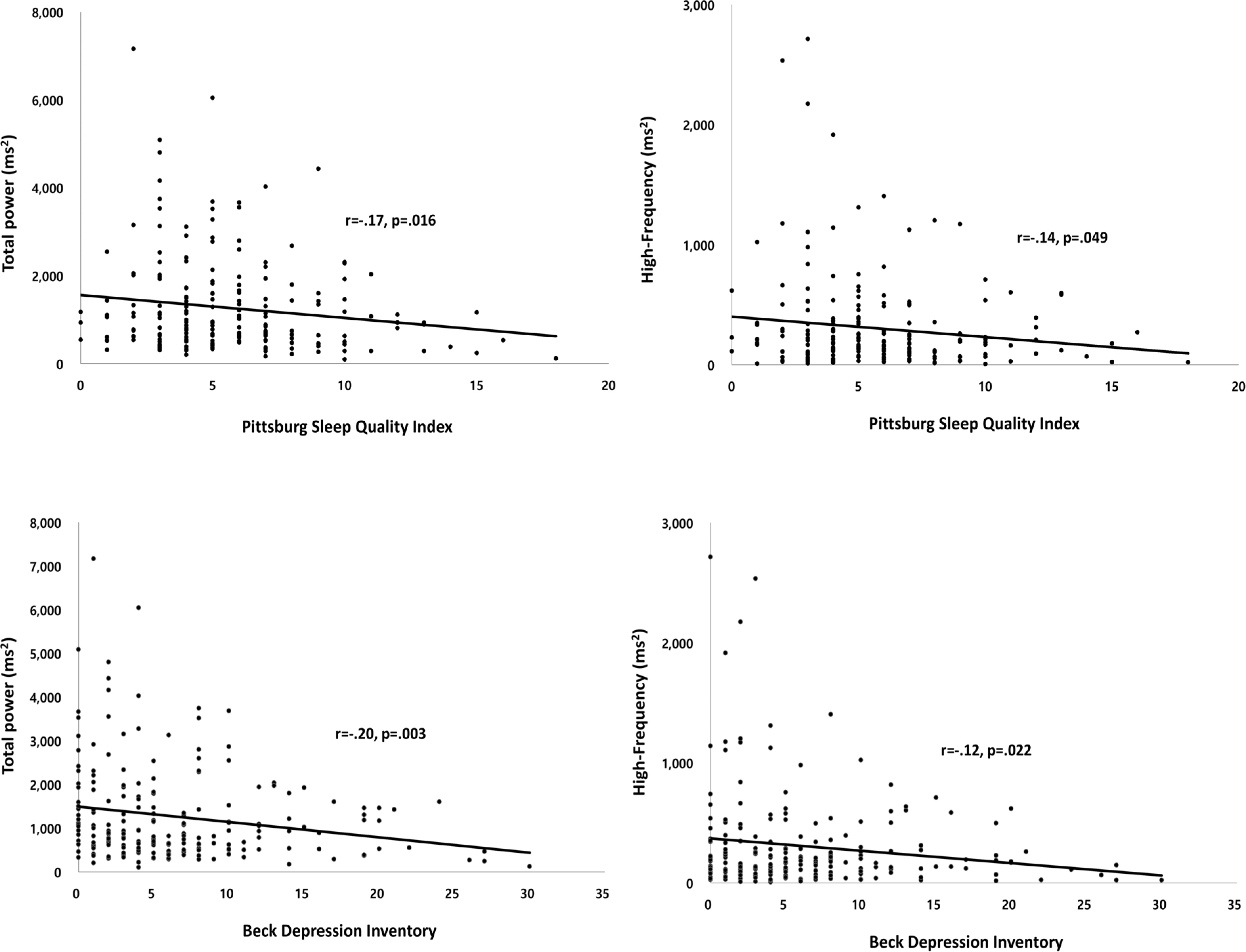
| Total power (ms2) | 1,295.38±1,133.08 | 1,432.50±1,294.56 | 1125.83±871.49 | 2.03 | .043 |
| LF (ms2) | 433.01±593.08 | 486.59±662.37 | 366.74±489.65 | 1.45 | .148 |
| HF (ms2) | 304.57±395.88 | 351.97±467.80 | 245.96±274.19 | 2.04 | .043 |
| LF/HF ratio | 2.72±3.94 | 2.56±3.44 | 2.93±4.50 | -0.67 | .501 |
| FSS | 2.94±1.41 | 2.59±1.23 | 3.37±1.50 | -4.08 | <.001 |
| BDI | 6.45±6.12 | 5.06±5.34 | 8.16±6.61 | -3.66 | <.001 |
| S-STAI | 36.78±8.89 | 35.75±8.89 | 38.07±8.78 | -1.88 | .062 |
| T-STAI | 39.62±10.43 | 37.20±9.55 | 42.61±10.74 | -3.84 | <.001 |
LF=low frequency; HF=high frequency; LF/HF ratio=low frequency/ high frequency ratio; FSS=fatigue severity scale; BDI=beck depression inventory; S–STAI=state-state trait anxiety inventory; T-STAI=trait-state trait anxiety inventory.
Correlations of Sleep Quality, Fatigue, Depression, and Anxiety
| Variables | PSQI | FSS | BDI | S-STAI | T-STAI |
|---|---|---|---|---|---|
| PSQI | 1 | ||||
| FSS | .39 (<.001) | 1 | |||
| BDI | .44 (<.001) | .37 (<.001) | 1 | ||
| S-STAI | .23 (.001) | .28 (<.001) | .59 (<.001) | 1 | |
| T-STAI | .34 (<.001) | .41 (<.001) | .69 (<.001) | .72 (<.001) | 1 |
PSQI=Pittsburgh sleep quality index; FSS=fatigue severity scale; BDI=beck depression inventory; S-STAI=state-state trait anxiety inventory; T-STAI=trait-state trait anxiety inventory.
Good sleepers=Pittsburgh sleep quality index score ≤5; Bad sleeper=Pittsburgh sleep quality index score>5; BMI=body mass index.
PSQI=PittsburGh Sleep Quality Index.
LF=low frequency; HF=high frequency; LF/HF ratio=low frequency/ high frequency ratio; FSS=fatigue severity scale; BDI=beck depression inventory; S–STAI=state-state trait anxiety inventory; T-STAI=trait-state trait anxiety inventory.
PSQI=Pittsburgh sleep quality index; FSS=fatigue severity scale; BDI=beck depression inventory; S-STAI=state-state trait anxiety inventory; T-STAI=trait-state trait anxiety inventory.